Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.
Overview
For many years wellness has been viewed from somewhat of a skeptical perspective. Intuitively, the value of health and wellness programs seems so obvious but for some reason the marketplace has not actively accepted and endorsed them. However, as the Bob Dylan song says “the times they are a changin’.” Health and wellness programs have gained respectability and many organizations are implementing and offering them to their customers and publics. This article provides a framework to evaluate health and wellness programs, determine whether or not they will be effective and determine whether or not they will effectively reduce and/or stabilize health care costs. We estimate that an effectively implemented health and wellness program can reduce aggregate health care costs by as much as, or possibly more than 20% – 30%. Also, these costs savings continue for more than one year. We expect health plans, providers, and employer plan sponsors will become even more interested in health and wellness programs once they see the significant financial benefit it can create for them.
Background
For more than 30 years much of the authors’ consulting efforts have been focused on the assessment of and implementation of highly effective care management programs having developed and designed some of the industry’s most widely used care management tools[1]. Most of our efforts have been focused on the efficient delivery of health care services (i.e., how to deliver high quality, cost-effective patient-centered care). Our overall vision also included both patient education and what has been called demand management, today most often called health and wellness. However, in the early to mid-1990s the market did not actively gravitate to these types of resources and our development plans were postponed.
Health plans, for the most part, were not convinced that employers really wanted health and wellness programs or would pay for them. Most employers did not have a long term perspective and were not excited about investing and implementing a resource that may eventually benefit their competitors as a result of employee turnover. Why invest in something where the benefits are generally long term and may not be actualized during the current leader’s tenure? They had a much shorter-term perspective and were much more interested in reducing their health care costs now, this year. As a result, they were often much more interested in care management techniques. After all, our studies showed that as much as 50% – 54% of inpatient services and as much as 25% – 35% of ambulatory services were potentially avoidable. Potential savings well over 30% were extremely luring.
Health care providers were and continue to be much more focused on delivering health care services (i.e., curative sick-care) rather than actively promoting wellness with their patients (i.e., true wellcare). Much of the time, many of the health and wellness promoters were often viewed as being outside the mainstream health care system, potentially aligned with fringe or alternative healthcare providers not accepted by traditional medical doctors. Yes, there were a few diehards actively promoting wellness and prevention, but they were a definite minority.
Much of what was promoted as wellness was not scientifically sound and was without measurable and beneficial outcomes. Individuals were caught in the middle not sure what they should think, what they should do, or whom to believe, oftentimes just continuing down the path they were already on. Wellness programs happened more by accident or as an afterthought rather than by strategic and quality planning.
Today the health care stakeholder focus has changed, it is much different. Unlike the prevailing view that care management principles are politically incorrect, even though substantial savings remain, it is now politically correct and even popular to promote health and wellness principles. Individuals and organizations are increasing their efforts and committing substantial resources to improve overall health and wellness. Individuals are increasingly responding to programs that improve their personal health and wellness. Health plans and plan sponsors, now less willing to promote managed care concepts have decided that they will encourage health and wellness with their customers and publics. The health and wellness momentum is growing and it is significant. Some employers now embrace not only the strategic long term benefit of such programs, but the short term impact of a “nurturing culture” where their employees feel cared for and valued. As they become aware of the significant savings potential for such programs, their interest escalates further.
The challenge with all of this health and wellness enthusiasm is answering the many tough questions facing the decision makers:
- how does one determine if a program works?
- which program works the best?
- how do you best implement a health and wellness program?
- what issues do individuals respond to the most?
- what characteristics assure or at least enhance the program’s success?
- how much money does a health and wellness program save?
- is it worth the effort (i.e., what is the ROI?)?
- are incentives effective in promoting change?
This paper will help provide tools to help answer these questions and provide a useful framework for future discussion.
The Change Management Connection
Health and wellness programs are really change management initiatives, focused on personal behavior change management, perhaps the hardest of all changes to make. Traditional change management focuses on moving an entity from its “current world” to a more desired “future world”. Current world in the health and wellness environment is the individual’s current health status. Future world is the hoped-for positive outcome of the health and wellness program (i.e., the individual’s ideal health status). The key ingredient to measure success is determining how to successfully transition the individual from today to the future, from their current world to their future world, from “interested” in true health and wellness to becoming genuinely committed.
It is helpful to look at this from two distinct perspectives: organizational change management and individual change management.
Organizational Change Management
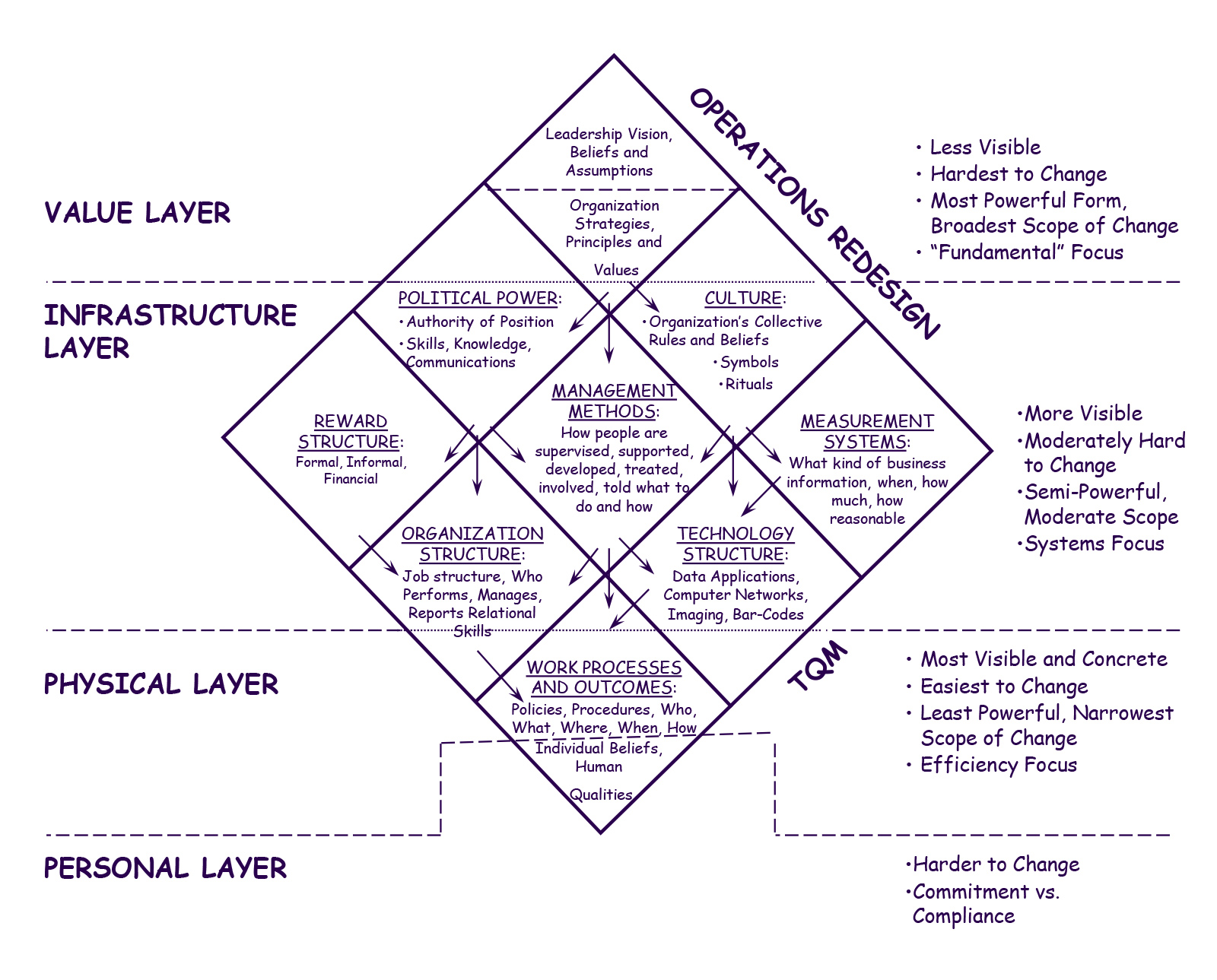
Classical change management principles offer useful ideas and concepts that can be directly applied to the organizational side health and wellness programs to better understand potential success and to design successful programs. A good example of this is shown in Exhibit A. This describes key factors in an organizational change management process. As Exhibit A shows, there are far-reaching factors that impact the success of the change management process including leadership, management methods, measurement methods, organizational structure, technology, etc. Only when all are appropriately considered will the organizational change management process achieve its goals. Exhibit A’s overlay of four layers with the individual pieces further demonstrates the forces which can disrupt the change management process.
Exhibit A: Organizational Change Management Grid[2]
Even the diamond shape of the change management grid is philosophically significant. Organizational and change management experts regularly use the management principle known as “tight-loose”. Exhibit A visually presents an extension of this “tight-loose-tight”. The first tight refers to a tightly defined vision/mission, one that everyone buys into. The second tight refers to a tightly managed execution or process. The loose refers to flexible design and organizational process. Note that the top of Exhibit A comes to a point (i.e., tight, narrow), the middle part is wider, and the bottom again comes to a point. Visually it demonstrates “tight-loose-tight”, which we believe to be the most effective approach.
In terms of Health and Wellness, both the organization’s programmatic health and wellness approach and the individual’s personal interaction with the approach (described in more detail later) can be described in similar terms to that presented in Exhibit A and be mapped to this grid to demonstrate the key success factors. If an organization designs the right strategic program for implementation, the individuals who are participating will respond accordingly. Historically, most health and wellness programs have focused on what the individual should do. The more ideal approach for organizations and individuals is to really focus on and develop the why and how considerations.
The most effective health and wellness programs are ones with the tightest vision and mission statement. This is where the program clearly identifies, incorporates and strengthens the appropriate motivations for change (“the why”). When an organization is truly committed to the process, amazing things can occur. Very specific and definite goals result in the best results. (i.e., Tight and non-negotiable).
Although it will be described in more detail later in this document, we believe a tightly defined health and wellness program vision should include the following three items:
- A Focused Program – a program that begins with a particular aspect of health and wellness, rather than trying to be everything to everybody
- A Hope-filled Program – a program that provides hope to participants, showing that it can be done and success is likely
- A Redemptive Program – a program that encourages participants who participate, motivates them along the way and incentivizes them to continue their transition. It is a program that gives “partial credit” for sincere participant efforts.
In addition, the most effective health and wellness programs incorporate a loose and flexible process or path. There are so many ways to structure and present programs, many with very similar results, that it is mandatory that the program incorporates flexibility. It is critical that the program tailor the specific application to best meet the needs of the individuals. Historically, this is where most of the narrow focus has occurred, rather than a “loose”, flexible approach. The exact structure and strategy (“the what”) need not be central in the context of genuine commitment and motivation. There is the capacity to customize and design specific strategies based on a host of unique and distinct considerations and preferences (i.e., Loose and flexible).
Finally, the most effective health and wellness programs have attracted highly committed individuals totally invested in the process (i.e., tight commitment). The sustained implementation (“the how”) is key for both short term and long term benefits and outcomes. Predictably, having the appropriate commitment in the context of a customized strategy can lead to the implementation of a process that will lead to lasting change and benefit (i.e., Tight and mandatory).
Unfortunately, we find that far too many health and wellness programs are structured Loose-Tight-Loose. There is a very loosely and poorly communicated program vision and goal, nebulous at best, combined with a rigid and tightly defined inflexible structure, and a loosely structured connection with the individuals resulting in less than desired results. A complex and rigid program presented in an apathetic environment will likely lead to extensive expended resources without much meaningful benefit. In contrast, a tight-loose-tight program has a much greater likelihood of success, far above the general programs seen today.
For example, certain weight loss programs provide a rigid manual with points and/or limits forcing people into cookie-cutter diet plans while doing little effective to grow commitment to the end goal. These are clearly loose-tight-loose programs. Yes, they oftentimes generate significant revenues to the sponsoring organization through membership and or meeting fees, with less than desired results and discouraged participants.
Individual Change Management
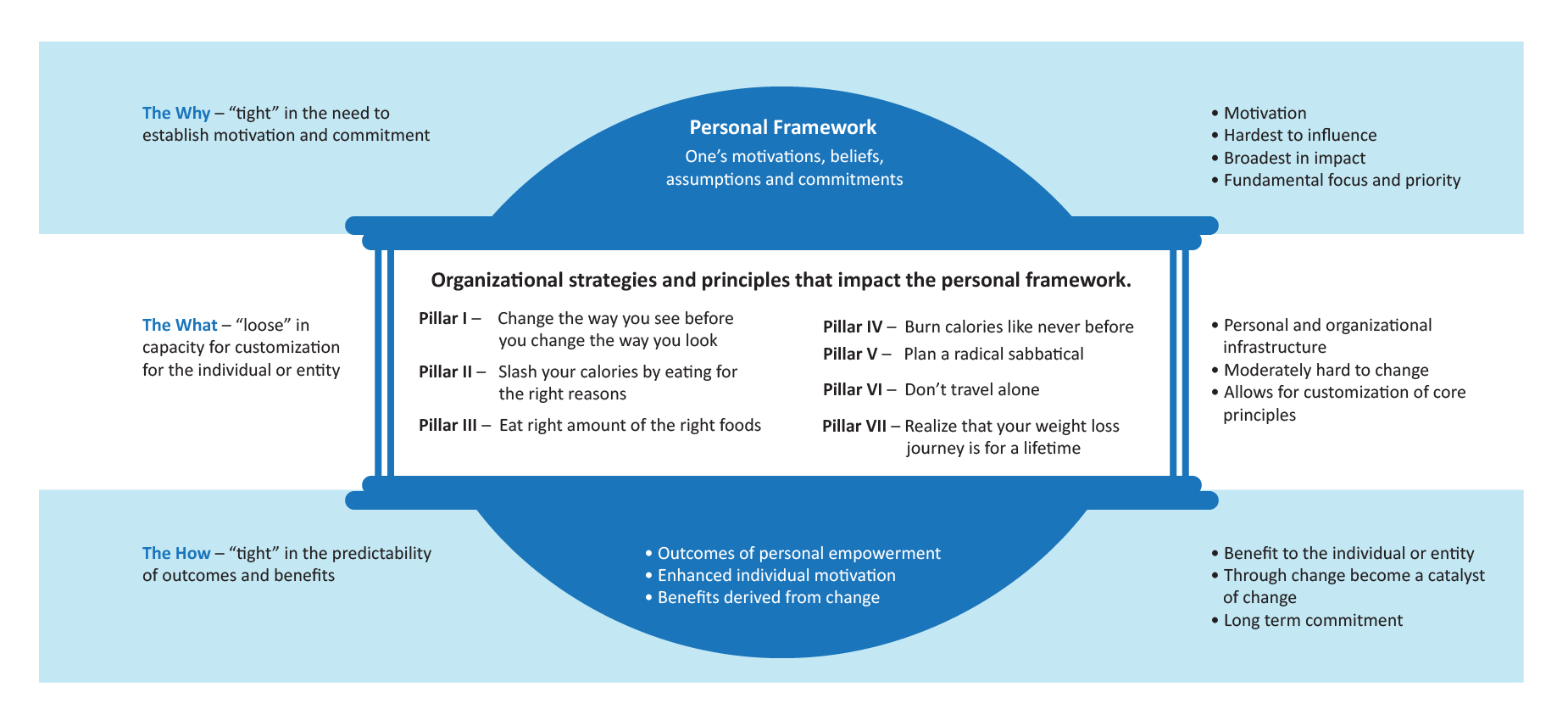
Just as with an organization, focusing on change management is key for any real impact to be made on one’s current health status. Whereas traditional health care, for the most part, focuses on treating illness and curing disease, true health and wellness programs will focus on individuals becoming more committed to changing their behavior and hence improving the quality and potential for a greater quantity of life. Personal change management principles offer valuable ideas and concepts that individuals can directly apply to improve the very quality of their lives. Exhibit B describes our model of the individual change management process. Just like with organizations, there are far-reaching factors that impact the success of a person’s journey into newfound health and wellness.
Exhibit B: AHP Health and Wellness Model
The egg shape of the personal or individual change management model is again philosophically and symbolically significant. Symbolically, unhealthy personal behavior often leads to carrying around extra weight around our midsections (i.e., egg-shaped physique). Philosophically, like organizational change, the proposed individual approach is a tight-loose-tight model but with gentler, softer edges and curves in comparison to the sharp edges of the diamond grid. The top of the egg, being the tightest refers to the need to have tightly defined personal motivation and commitment. The second tighter region at the bottom of the egg refers to the tightly defined outcome of personal empowerment. The larger, “loose”, wider middle of the egg model refers to the customized and flexible design of a personal approach that encompasses certain core healthy pillars that anyone can adopt into the context of their lives. Exhibit B comes to a point of sorts at both ends with a large wider middle area which visually demonstrates the tight-loose-tight of personal change management.
In terms of personal Health and Wellness, an individual’s personal approach can be mapped to this model to demonstrate the key success factors. Just like with an organization, most individuals respond in a very similar way. Most adults who are relatively informed do not just need to be told “what” to do. They may already know at various levels. What they do need the most is the support, encouragement and accountability to just do it. What they need is the inspiration and hope to know it’s possible. Too many times we focus on instruction and neglect inspiration. We prioritize giving people help without adequately providing a sense of hope that change is possible. We emphasize technique and neglect motivation. The ideal approach to individual change management is one that develops motivation, develops sincere commitment to the process, develops hope for the potential that it can be done and builds inspiration about the consequences of it actually occurring.
On the personal or individual level motivation is key! What often is lacking is appropriate and meaningful motivation which translates to a greater sense of commitment. The concepts of health and wellness change are not that complicated. It’s the application of simple principles into the complexity of an individual’s life which takes thoughtful and strategic consideration. The tight-loose-tight structure directly applies here. The individual needs to clearly know (i.e., tight):
- Why am I part of this program?
- What is the end goal or outcome?
- What will I achieve?
- What are the benefits of me participating?
- How much personal effort it will take? Too often this is inadequately presented and high recidivism or failure rates result from not buying in upfront to what will likely occur.
- What is the required process to be successful?
- What are my chances of success?
- Is this program clinically sound? What are the program’s credentials?
On a loose perspective, the individual needs to know what specific rewards or incentives are involved. Whether personally established by the individual or part of the overall program structure, the participant must value the rewards and let these motivate them in their transition process. There is a wide variety of incentives that could be used and uniquely tailored to each individual. Different individuals respond to different incentives, are motivated differently, and will perform differently. The program needs to react to these different perspectives.
Measurement systems are key to the individual, but their precise structure is less important. The individual needs to see that they apply to their lifestyle and normal thinking process. They have to be comfortable with what is going on.
On the bottom tight perspective, the individual needs to be closely held accountable and encouraged to continue the process they have begun. Without this the individual may give up, stop the program, lose heart and assume it is hopeless.
An Ideal Health and Wellness Program
Based upon our actuarial analysis we find that as much as 75% – 85% of the potential savings from health and wellness programs can be directly attributed to six specific and objectively measured factors:
- Obesity (i.e., as measured by the BMI or Body Mass Index)
- Fasting blood sugar
- LDL cholesterol (i.e., bad cholesterol)
- Blood pressure
- Smoking/non-smoking, and
- Personal fitness
Ironically, all of them with the exception of smoking/non-smoking are directly related to BMI. As individuals solve their BMI problem, they gradually solve most of their other problems. Some individuals with a genetic predisposition to certain conditions may require ongoing medications to keep one or more factors in control, but the vast portion of problems can be significantly improved and eliminated by eliminating obesity and achieving an ideal BMI or by at least improving it and moving closer to the ideal level. This suggests that significant gains can be made by creating a BMI-focused health and wellness program. Since smoking/non-smoking is somewhat independent, perhaps a two-pronged program (i.e., BMI and smoking cessation) is the best way to implement a program. This “tight” focus enables the program to quickly succeed, where other “loose” focus programs have failed or had significantly fewer results.
Although the actual results are significantly impacted by characteristics of the studied population (i.e., the population’s average BMI scores and the proportions of smokers to non-smokers), we find that in a fairly typical population overall health care costs can be reduced by as much as and possibly more than 20% – 30% if each of the individuals in an overall population advance to their ideal health status. On an individual by individual basis, the cost reductions on some are much more than this. A tangential benefit of this improvement is that the cost savings continue to occur for many years, not cost savings in just one year.
Every health and wellness program needs reliable ways of accurately measuring the program’s effectiveness. Each of the above six factors can be objectively measured through relatively inexpensive means. For example, a simple blood test can be used to measure blood sugar or LDL levels. Blood pressure can easily be measured by a trained individual or even by automated machines. Fitness can be broadly defined as the ability to function efficiently and effectively, to enjoy leisure, to be healthy, resist disease and to be able to cope with emergency situations. The health related components of physical fitness that could be measured include body-composition, cardiovascular fitness, flexibility, muscular endurance and strength. There are various ways to measure fitness depending on available resources and facilities. There are several available Health Risk Appraisal (HRA) packages that can give a report that incorporates both objective measures as well as subjective responses to a set of questions.
As mentioned earlier, it is also critical to provide hope to the participants. A believable example or champion is always beneficial to motivate participants. One interesting example of this is one of the authors of this article.
Nicholas J. Yphantides, MD, Dr. Nick as he is known, the author of “My Big Fat Greek Diet”[3], used to weigh 467 pounds, has lost more than 270 pounds and has successfully kept it off for almost seven years. His significant and relatively quick weight loss journey is chronicled in the book. Dr. Nick outlines Seven Pillars of Weight Loss Success, which are critical to successful weight loss and are integrated in the Individual Change Management Model. They can be summarized as follows:
Pillar I: “Change the way you see before you can change the way you look.” As discussed change is at the core of what is needed but rather than focusing on changing specifics first one has to undergo a change in their perspective which will naturally lead to a change in habits and behavior.
Pillar II: “Slash your calories by eating for the right reasons.” Way to much focus is spent on diets and what to eat. Critical to healthy living is having a healthy relationship with food and rediscovering its role as fuel and not as a means of dealing with any number of other personal emotions or needs.
Pillar III: “Fill your tank with the right amount of the right foods.” Rediscovering an appropriate sense of satiety by responding to the body’s signals and as a result, eating an appropriate amount of the right kind of food is core to learning how to eat to live healthily.
Pillar IV: “Burn calories like never before.” It is imperative and necessary not only to lose weight but not to rediscover it again once lost (i.e., gain it back). As individuals become more physically active they will keep it off. Strategies to have fun and pleasure burning calories are important for it to be a sustainable habit.
Pillar V: “Plan a radical sabbatical.” Most need to take some kind of a break from the routine if we are going to establish a healthier lifestyle. Combining pleasure and benefit and carving out time that one can focus on their health as a priority for lasting vitality is core to successful weight loss.
Pillar VI: “Don’t travel alone.” The assumption is that this is an ongoing journey for most. There are times where initial momentum is present but for many, the notion of support, encouragement and some level of accountability are going to be key factors to long term success. It is so important to people committed to the group nature of accountability and healthy co-reliance on healthy living.
Pillar VII: “Realize that your weight loss journey is for a lifetime.” Many people see weight loss interventions as a temporary lifestyle modification where in reality it is a life long commitment to a new set of habits and behaviors. It’s not about losing weight. It’s about losing it and not rediscovering or finding it again that really counts.
Weight loss programs (i.e., BMI improvement programs) aligned with these key principles have demonstrated much greater success than those missing these. Most current efforts fall short of lasting impact in that they target the stomach. Many overweight people who have health-related consequences for their extra weight do not have a problem with their stomachs as much as they do with their “heads and hearts.”
Focusing first on those with BMI concerns accomplishes the greatest value in the health and wellness program. Dr. Nick’s approach proves to be quite effective in making those changes. The second focus is on those currently smoking, using traditional smoking cessation programs and interventions. This approach could be called wellness triage, focusing on those who need it the most. The prioritization in such a program is as follows:
- BMI improvement
- Smoking Cessation
- Blood pressure reduction and control
- LDL reduction and maintenance
- Fasting blood sugar reduction and maintenance
- Fitness improvement
Integration with Health Benefits Program
The above health and wellness approach can be further enhanced through the integration of it with the health benefits program. Combining an organization’s change management model along with the individual model could lead to a radical transformation in the workplace and the individual’s lifestyle. Several approaches can be used to effectively accomplish this, however, one popular approach is linking the six key health status indicators to a health and wellness points system, and then linking the points system to a particular benefit level.
One example of how this could be implemented is as follows:
- 20 points allocated to each of the six metrics
- Full points are credited when the covered individual achieves ideal levels in each category (e.g., BMI <= 25, fasting blood sugar <=100, etc.)
- Partial credit is given for participation in programs enabling the individual to improve their measures (e.g., approved smoking cessation program, approved weight loss program, etc.)
- Different points are given for different progress within each category’s ranking process (i.e., 5 points for specific BP range, 10 points for another, 15 points for a third, etc.)
- Once a year each individual around the time of the open enrollment gets a blood test and physical exam through their family doctor with scores reported to the administrator. As part of the process, the benefits administrator provides each employee with a voucher to pay the provider directly.
- Where more than one individual is covered under the contract, the average score is calculated for all covered individuals.
- The wellness points are accumulated to calculate a wellness score.
- Perfect performance on all six metrics would result in a score of 120.
- Four separate ranges of scores are set up (i.e., <25, 25 – 49, 50 – 74, 75+). Each range identifies what type of plan the employee is eligible for. The employee can buy up to a better plan but for the same contribution is eligible for the plan suggested by their wellness points.
- Benefits are identical in each plan, the only difference is the deductible. The individual can reduce their out of pocket by improving their health status.
This type of program is built around the concept discussed earlier:
- Incentive driven – the better the wellness scores the lower the deductible, best benefits are given even if one bad area (i.e., 120 total vs 75+ category)
- Redemptive – gives partial wellness credit to those who are trying.
- Hope-filled – wellness program built around concepts that work
- Focused – BMI centric with wellness triage.
Programs of this kind must consider federal anti-discrimination regulations. It is our understanding that current regulations permit health and wellness programs which reduce deductibles/copays for improved health status. Regulations impacting this are continually changing and it is critical to keep this in mind when designing such programs.
Summary
Wellness programs can be established in many different ways. As health plans and plan sponsors decide to impact the wellness of their customers, the programs must achieve the financial success they were intended to get. The above information provides one effective approach that could be used and a framework to assess different programs. Since so much change is happening today, it is important to track these issues very closely to assure the greatest health cost savings possible.
There is a significant potential for health cost reductions from appropriately implemented health and wellness programs. Not every program will be able to achieve the entire 20% – 30%, however, in the current economy, a minimum savings of 5% – 10% would be significant to most health care planners. Additional savings can be achieved if health and wellness principles are strategically combined with effective care management principles.
Endnotes
[1] While at Milliman & Robertson, Inc., now Milliman, Mr. Axene and his consulting practice were responsible for developing the Milliman Care Guidelines. While also at Milliman, Dr. Liliedahl was the Care Guideline’s Chief Medical Officer and author of two of the firm’s initial guideline products.
[2] Change management grid initially developed by Dutch Siedentopf, change management consultant.
[3] Yphantides, Nicholas, “My Big Fat Greek Diet”, Nelson Books, 2004, ISBN 0-7852-6025-0
About the Author
Richard Liliedahl, MD, is the Chief Medical Officer of Axene Health Partners, LLC and is based in AHP’s Temecula, CA office.