Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.
Introduction
Today most health care discussions focus on health care reform with an emphasis on financing and access. Few will disagree, though, that healthcare costs in the United States are an increasingly costly burden. A key contributing factor to those rising costs is often ignored in reform discussions: the impact of chronic diseases.
In 2010, 75% of US healthcare spending was for the direct care of chronic diseases1 like heart disease, cancer, diabetes and pulmonary diseases like COPD and asthma. Although some of the risk factors for chronic diseases, like aging and genetics, cannot be changed or modified, others, like smoking and obesity, can be modified. Americans are able to reduce our overall healthcare costs by reducing these risk factors. For example, studies indicate that a 5% decrease in obesity rates could result in savings over $29 billion.2 While the ultimate responsibility for the diagnosis, treatment, and prevention of disease lies with the patient and his or her doctor, there are several third party and public health organizations providing valuable support to these efforts. It is expected that the 2018 budget for one of the key third parties, the Department for Health and Human Services, will be significantly reduced.3
This article further explores the impact of chronic diseases on the healthcare landscape in the United States, discussing the key modifiable risk factors and opportunities for prevention and improved care management.
The Cost and Prevalence of Chronic Diseases
Half of all Americans have at least one chronic disease, like diabetes, cancer and heart disease, and almost a third have more than one condition. For adults, the most prevalent condition is heart disease. For children, the most common conditions are asthma and allergies.4
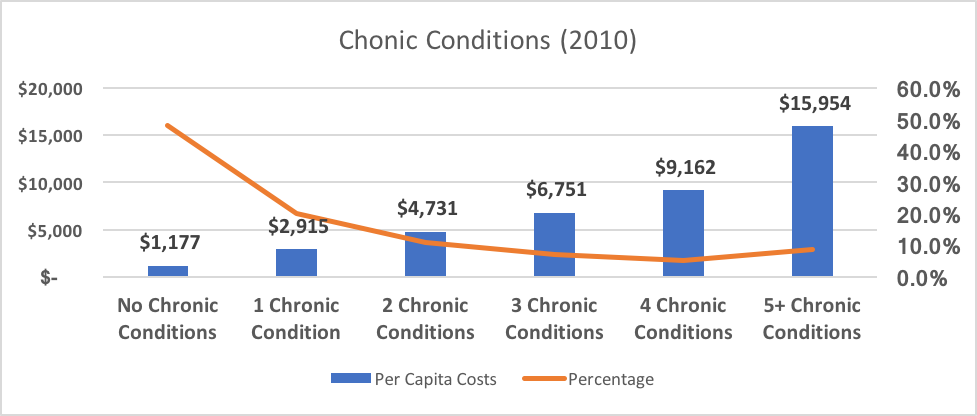
The average healthcare cost per person varies by the number of chronic conditions the person has, as shown below in Table 1 below. The average cost for a person with just one chronic condition is over twice as high as person with no chronic conditions, and the average cost for a person with 5 or more conditions is over 13 times as high.5
Table 1
People with 5 or more conditions account for less than 9% of the population, but nearly 35% of total costs.6
The burden of chronic diseases goes far beyond the direct amounts spent on these diseases. In the U.S., 7 out of every 10 deaths are caused by chronic diseases each year.7 Additionally, there are indirect costs through lost productivity and unmeasurable losses in the quality of life and the ability to perform activities of daily living like bathing and eating.
Modifiable Risk Factors
Risk factors are conditions or lifestyle choices that make a person more likely to develop a disease or to develop complications from a disease. Some risk factors for chronic diseases, like aging and family history, cannot be changed or modified. There are, however, a small set of modifiable risk factors largely responsible for many chronic conditions.
Smoking
Smoking is the modifiable risk factor that has received the most attention over the last 50 years. This push began in 1964 when the Surgeon General released a report on the dangers of smoking. As a result of this report, and a follow-up report on the dangers of second-hand smoke, there was a huge push to reduce the number of smokers. Efforts included ads on the danger of smoking sponsored by both governmental organizations, like the Centers for Disease Control and Prevention (CDC) and non-governmental organizations (NGOs) like the American Heart Association and the American Cancer Society. Eventually, these efforts were supplemented with health-plan sponsored smoking cessation programs and a variety of legislative actions like smoke-free buildings, cigarette taxes, and banning cigarette ads on television. As Table 2 below shows, these programs have been successful in reducing the number of smokers. In 1965, 42.4% of all adults were smokers. Today that number is 15.1% – a 64% drop.8
Table 2
Although these results are impressive, smoking is still a major problem in the United States:
- Cigarette smoking is still the leading cause of preventable diseases and deaths in the United States. About 480,000 deaths each year are attributed to cigarette smoking, which equates to roughly 1 in every 5 deaths.9
- On average, people who have never smoked live a decade longer than smokers.
- The estimated economic costs attributable to smoking and exposure to tobacco smoke is approaching $300 billion annually, with direct medical costs of at least $130 billion and productivity losses of over $150 billion.10
- Smoking causes colorectal and liver cancer and increases the failure rate of treatment for all cancers.11
There are some concerns that evidence-based, proven tobacco control interventions, like hard-hitting media campaigns and excise taxes, are underutilized. In addition, several new end-game strategies, like reducing the nicotine yield to non-addictive levels, have been proposed to help reduce smoking rates even further. Yet, these two strategies would require legislative changes.
This increase has taken place in spite of the fact that, as with smoking, there are many community outreach programs in place throughout the country.
Obesity
Over the past decade, another risk factor, obesity, has also received a lot of attention. Obesity is a proven risk factor for type 2 diabetes, heart disease, hypertension and some types of cancer. Currently, estimates for the costs associated with obesity range from $147 billion to $210 billion per year. In addition, it is estimated that obesity costs employers about $506 per year for each obese employee due to absenteeism and loss of productivity.12
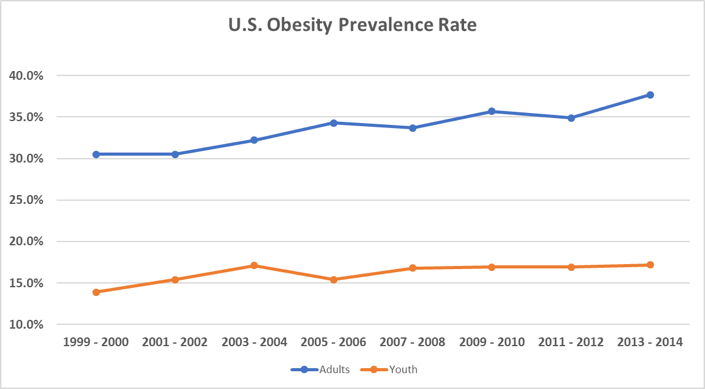
Unlike smoking, though, obesity prevalence rates continue to rise as shown in Table 3.13 This increase has taken place in spite of the fact that, as with smoking, there are many community outreach programs in place throughout the country.
Table 3
In part, this impact difference is because obesity is caused by a combination of factors, including behavior, genetics, and socio-economic factors. Also, community outreach programs, are typically educational in nature: they create awareness of a problem, like obesity, and they provide valuable nutritional information. However, there is much more involved in making long-term behavioral changes than simply being aware of the problem. Once someone is motivated to make healthy changes, they need support, encouragement, and accountability, all of which are provided through community channels (whether community is family-based, employer-based, church-based, government-based, etc.). Many employers, especially those with over 200 employees, now offer employee wellness programs to provide support and, in some cases, financial incentives.14 Although there is considerable debate on the effectiveness of these programs, one reputable study showed that for every $0.50 spent on a lifestyle management program, the return on investment was $6.00 per member per month.15
Legislative activities also play a role. Many countries, as well as a few U.S. localities, now tax sugary drinks in an effort to curb obesity. According to a World Health Organization report, a tax of 20% on sugary drinks can lead to a reduction in consumption of around 20%.16
Disease Management
Early detection of chronic illnesses can make a considerable difference in the resulting costs, both from a personal and a dollar perspective. For example, treatment of early stage breast cancers costs about $11,000 but breast cancers diagnosed at a later stage average around $140,000 in costs. But, even after a chronic condition has been diagnosed, lifestyle factors have a significant impact on limiting progression or complications of the illness, in addition to adhering to any prescribed medication. Regular office visits and tests are scheduled to make sure the patient stays on track with their overall treatment plans.
Historically, insurers have provided considerable support to the patient and to the doctor to manage the care of chronic illnesses, including:
- Disease management programs that provide individuals at risk with education and other support need to prevent a disease or minimize complications
- Low cost-sharing provisions on medications and other services with a proven record of keeping a condition under control
- Reimbursement methods that reward providers based on outcomes and quality, not just on service provided
- Care coordination programs designed to minimize inpatient length-of-stays and re-admissions
The clinical community is also actively working on improving chronic disease management by developing optimal treatment guidelines using evidence-based medicine. In addition, they are looking for new technologies that help to enhance quality of care and/or reduce cost, such as:
- 3-D mammography designed to reduce the number of false positives and missed breast cancers
- Telemonitoring techniques for real-time testing for biometrics like blood pressure. These will allow professionals to detect problems as they occur and allow for necessary care.
- 3-D organ printing which should reduce both costs of organ transplants and waiting times.
We can also expect to see a number of new, albeit costly, drugs in the market place to improve outcomes for chronic diseases. For example, there is a new drug, pembroluzimab, which is effective in treating cancer if genetic testing reveals defects in so-called mismatch repair genes. However, this drug is expected to cost around $100,000 per year per patient.17
Public Health Support
Historically, the Department of Health and Human Services (HHS) has played a key role in controlling diseases in general. For example, the Centers for Disease Control and Prevention (CDC) has coordinated efforts to reduce factors at both the individual level, by providing health care interventions, and at the population level, by promoting policies and environments that promote health. In addition, the CDC has provided a surveillance system used to track results. Another important agency is the National Institutes of Health (NIH), which performs original research and coordinates many of the efforts to define clinical guidelines.
Currently, the 2018 HHS budget is expected to be cut by about 18%. Although a thorough review of the budget is out-of-scope for this article, it does appear that additional money will be going to states as part of block grants. Specifically, the CDC is allocating $500 million to America’s Health Block Grant Program, which is designed to increase flexibility for state and tribal efforts to fight chronic disease.18
It may take several years before the impact, if any, of these funding changes on the chronic disease burden will be known. We do know, however, that several NGOs are stepping up their efforts to combat chronic diseases. For example, the American Diabetes Society is actively promoting increased spending by both the federal government and private organizations (such as the biotechnology industry) in order to reduce costs related to diabetes care.19
Conclusion
Clearly, chronic condition diseases significantly contribute to the ever-increasing US healthcare costs. There could be substantial savings to the American system if we reduce the prevalence and complications of these illnesses through some combination of prevention and disease management. This will not be easy. There are many players involved, including the clinical and scientific community, state and federal governments, NGOs, and, most importantly, individuals.
1AHRQ, https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf
2http://www.ncsl.org/research/health/diseases-and-conditions/obesity.aspx
3HHS, https://www.hhs.gov/about/budget/fy2018/budget-in-brief/index.html
4AHRQ, https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf
5Ibid
6Ibid
7https://www.cdc.gov/chronicdisease/overview/index.htm
8https://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm
9https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm
10https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm
11https://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf
12https://www.cdc.gov/chronicdisease/overview/index.htm
13https://www.cdc.gov/nchs/data/databriefs/db219.pdf
14http://www.kff.org/health-costs/report/2016-employer-health-benefits-survey/
15http://www.rand.org/content/dam/rand/pubs/research_briefs/RB9700/RB9744/RAND_RB9744.pdf
16http://apps.who.int/iris/bitstream/10665/250303/1/WHO-NMH-PND-16.5-e
17https://www.cdc.gov/chronicdisease/overview/index.htm
18https://www.cdc.gov/budget/documents/fy2018/fy-2018-cdc-budget-overview.pdf
19http://main.diabetes.org/dorg/PDFs/american-diabetes-association-strategic-plan-2017-2020.pdf
About the Author

Joan Barrett, FSA, MAAA, is a consulting actuary with Axene Health Partners, LLC and is based in AHP’s New England office.