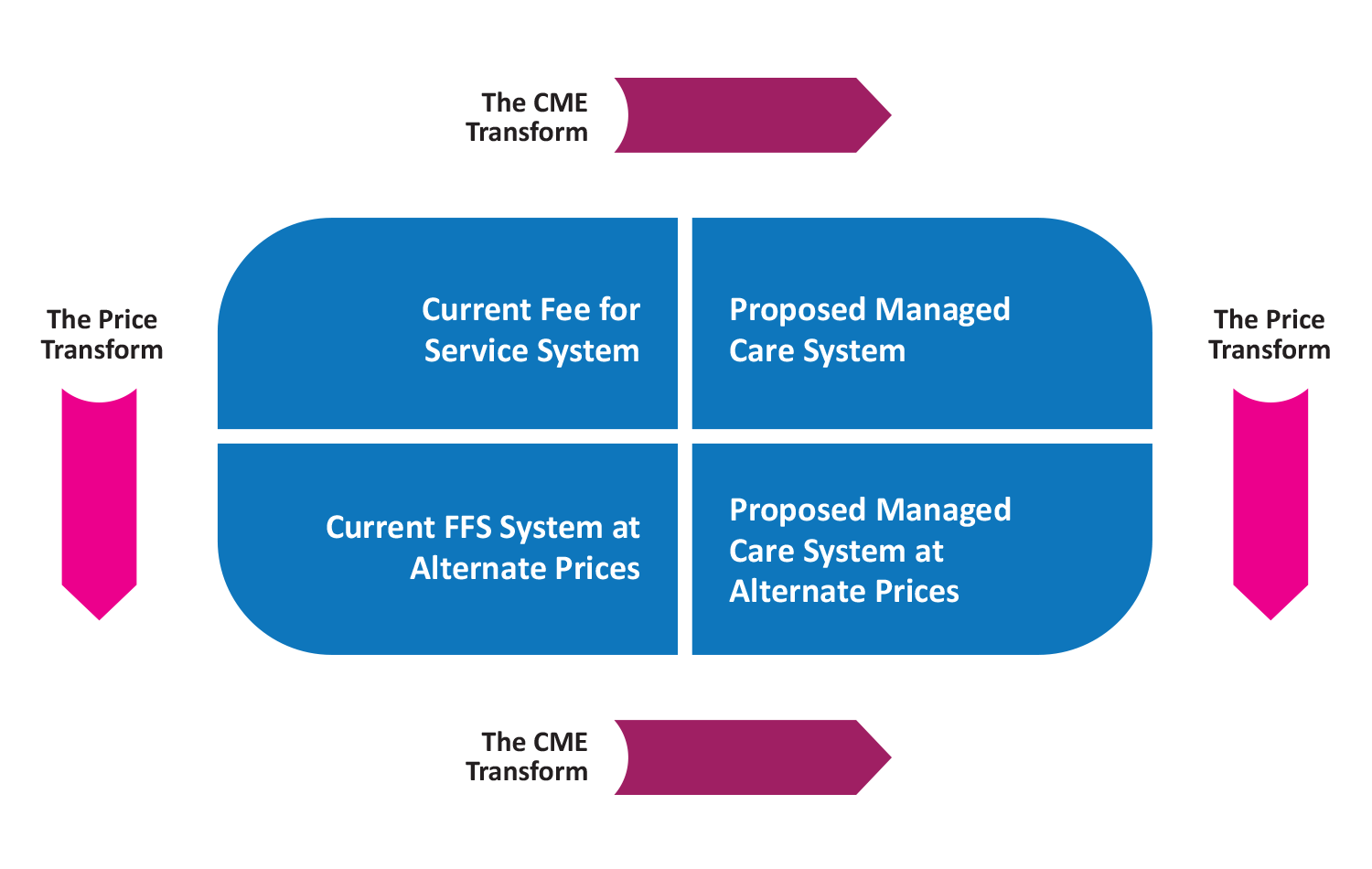
Students of mathematics are familiar with the concepts of transforms or transformations (e.g., LaPlace or Fourier transforms). Essentially these are tools which help mathematicians better understand complex functions and formulas. There is a nearly equivalent concept in health care that we will discuss in this article. I have found it quite useful in explaining and understanding health care. As the market moves to more of a population health approach, this will become increasingly important. The following diagram helps introduce the transformation process.
The transformation process begins in the upper left-hand corner. The current delivery system has specific characteristics, its own level of utilization and reimbursement scheme. As prices for services are modified the “Price Transform” occurs. This might be the result of a fee discount, the application of some specific fee maximum, or the use a specific fee schedule (e.g., Medicare RBRVS).
The second transformation occurs when care is impacted by a new and improved care management process (i.e., perhaps the implementation of evidence based practice guidelines or care management oversight). Patterns of care observed in the Current FFS system may change or perhaps become more efficient. The characteristics of this change is referenced by the upper right-hand corner. If those changes are similarly applied to the delivery system described in the bottom left hand corner, we transition to the bottom right corner.
As we move from the “current” system to the “proposed” system, we identify two major transformations we need to consider:
- How much different will the expected reimbursement be?
- How much different will the expected utilization patterns be?
In the chart above the transformation can be down and right or right and down. We get to the same point, a delivery system that is different from what we have today with changes in reimbursement and utilization.
Actuaries often present the delivery system characteristics in terms of what is known as an actuarial cost model. A robust model shows utilization information, unit cost information and resulting health cost information in terms of per member per month (PMPM) costs. Utilization is usually described in terms of utilization per 1,000 members. Unit costs are described in terms of cost per unit of service. This information is presented for a wide variety of categories including hospital inpatient, hospital outpatient, primary care, specialty care, pharmacy, etc. Detailed cost models may have as many as 50 – 100 categories.
The Price Transform demonstrates the impact of the change in payment rates. The simplest Price Transform transitions the model from Billed Charges to some agreed upon typical charge level. For example, this might be the health plan’s allowed charge level, or Medicare payment levels, or even Medicaid payment levels. In the case of capitation, it might be the fee-for-service equivalent payment level. The amount of the Price Transform is often described as reflecting an X% discount (the ratio of the proposed to the current payment rates).
Observations show that close to two-thirds of the overall cost of avoidable care is hospital inpatient based. As a result of this, most of the care management activities are focused in inpatient care.
The CME Transform references the change in what we call Care Management Effectiveness (CME). CME is a measure of how effective the care management process is. CME is a spectrum ranging from 0% to 100%. A CME score of 0% suggests nothing is being done to impact the behavior of providers or an ineffective care management program. A CME score of 100% suggests everything is being done that could be done and providers are performing at optimal or best-in-class levels. The best-in-class health care systems operate in the 85% – 95% CME level. More common operating results are in the 60% – 70% range. As CME increases the cost of the system declines as potentially avoidable care is eliminated from the system. Since health care outcomes cannot be perfectly predicted, there always is a residual of potentially avoidable care in even the best system. Observations show that close to two-thirds of the overall cost of avoidable care is hospital inpatient based. As a result of this, most of the care management activities are focused in inpatient care.
As the focus of health care change moves towards population health and its related efforts, it will become increasingly important to understand these two transforms and how they can be both managed and measured. It critical that we understand both financial effect and the impact on quality. One of the claims of those endorsing population health methods is the favorable impact on the cost of care. These transforms help to quantify the impact of various methodologies and approaches.
Fortunately, actuaries have developed very useful tools to accomplish this analysis and can add significantly to the discussion. These tools, including the actuarial cost model, can be used to predict the impact on the overall cost of the proposed delivery system. A couple of sample questions easily answered by these approaches are:
- What would be the financial impact of transitioning today’s employer based health care to a system utilizing Medicare payment rates?
- How much would the overall US health care system cost if we could implement a common and highly effective care management system?
The first question essentially considers the Price Transform. Once we know the relationship between typical payment rates and Medicare, we can apply the Price Transform to the cost of the current employer based health care system to pursue an answer to this question. We would also need to assess the impact to the CME Transform of this type of fee reduction (i.e., additional utilization increases resulting from reimbursement reductions). A simple version of this could be accomplished by comparing the average payment rate in the current system expressed as a percentage of Medicare payment levels. If current payment rates are 150% of Medicare, moving it to Medicare could potentially reduce costs by one third (i.e., 100 / 150 = .667). This obviously assumes that there would be no utilization increases as a result.
The second question considers the CME Transform. This requires an analysis of the current CME score for major sectors of our health care system and compares it to the most likely CME score we could achieve. Each of the health care system markets could be analyzed and combined to achieve an overall impact. If today’s composite CME score is 60%, an improvement from a 60% CME score to a 90% CME score could substantially reduce the expected cost of health care. The savings is derived from the actuarial cost models consistent with both the 60% and the 90% delivery systems, not from the ratios or CME scores themselves. The projected savings are substantial suggesting reductions of at least 15% – 20%, perhaps as high as 25% – 35%.
The use of these two transformation concepts is and has been valuable for many years. It provides an easy to understand structure to evaluate alternative approaches and methodologies.
Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.