Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.
Introduction
As health costs spiral out of control, health plans and plan sponsors are starting to experiment with new and innovative solutions to constrain the undesired escalations in cost and perhaps improve the outlook. The market is desperately looking for hope. For many years, the author has described the cost control mechanisms as the “three legged stool”. The visual below shows this.
If, and when, the providers are reimbursed appropriately with the right incentives (i.e., the left leg), health care services and providers are effectively managed (i.e., the right leg) and appropriate benefits are offered (i.e., the center leg), only then will the system will be the best it can be (i.e., the “Success!” outcome) with the lowest health care costs and the highest quality. This approach has worked well to focus health plans and providers, but the market expects more. Something more is needed.
An emerging perspective, one that will be described in this article, is user-centric health benefit design. This approach, when implemented successfully, propels the organization to new performance opportunities above and beyond prior results. The combination of a robust analytics-driven understanding of who is making the key health care decisions (i.e., the individual) and what their intrinsic behaviors are provides valuable new information to improve cost control efforts.
Personas and Archetypes
Personas are the “who” of a population. Personas are often defined by the demographics of the population (i.e., age, gender, income, occupation, interests, geographic region, etc.). The linkage of both historical claims data and what is known as “big-data” (i.e., consumer behavior information) can expand the health plan’s or plan sponsor’s understanding of the personas to show many interesting characteristics of this population. This aggregated data can be used to segment the population into distinct persona categories each with special health care needs and individual purchasing behaviors. The information is useful in designing and targeting specialized benefit designs and products for each of the personas. The population without claims or with very few claims can be categorized to specific persona using just their demographic information.
Where personas focus on “who”, Archetypes focus on behavior. They describe who does what, when do they do it and why did they do it. This is like an exit poll at an election (i.e., who did they vote for and why). Archetypes help explain behavior patterns and what drives different individuals to certain behaviors. They are useful in determining what action will result in a specific response. When thoroughly investigated they can be used to develop specific product features.
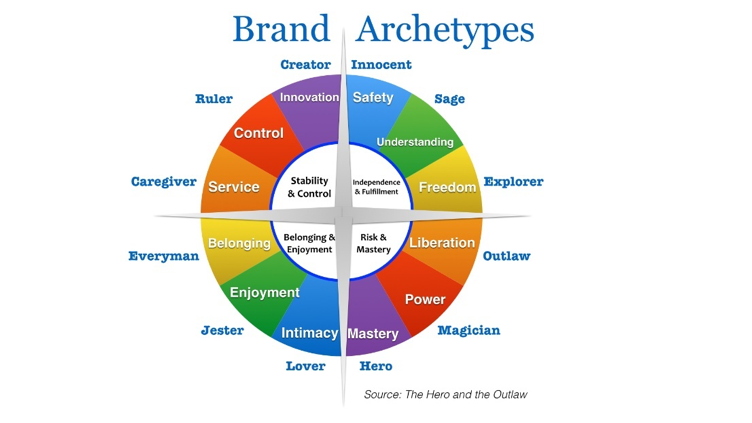
Archetypes were used in ancient Greek times. Carl Jung used the concept in his theory about the human psyche. Jung developed 12 major archetypes as shown in the following diagram.
These can be grouped into four sets of three architypes based upon their individual characteristics. The following table elaborates on these summarizing each of them in more detail.
| Archetype | Motivation | Motto | Core Desire |
| Creator | Stability & Control | If it can be imagined, it can be created. |
Create something of enduring value. |
| Caregiver | Stability & Control | Love your neighbor as yourself. |
Protect people from harm. |
| Ruler | Stability & Control | Power isn’t everything. It’s the only thing. |
Control |
| Jester | Belonging & Enjoyment | If I can’t dance I don’t want to be part of your revolution. | To live in the moement with full enjoyment. |
| Regular Gal/Guy | Belonging & Enjoyment | All men and women are created equal. |
Connection with others. |
| Lover | Belonging & Enjoyment | I only have eyes for you. | Attain intimacy and experience sexual pleasure. |
| Hero | Risk & Mastery | Where there’s a will, there’s a way. |
To prove one’s worth through courageous and difficult action. |
| Outlaw | Risk & Mastery | Rules are meant to be broken. | Revenge or revolution. |
| Magician | Risk & Mastery | It can happen! | Knowledge of the fundamental laws of how the world or universe works. |
| Innocent | Independence & Fullfillment | Free to be you and me. | To experience paradise. |
| Explorer | Independence & Fullfillment | Don’t fence me in. | The freedom to find out who you are through exploring the world. |
| Sage | Independence & Fullfillment | The truth will set you free. | The discovery of truth. |
The archetypes can be used in concert with key product features to drive specific behavior. In the case of health care benefit plan design, the plan design can be designed to match the needs of various archetypes evident in the underlying population. For example, Hero and Outlaw are both archetypes in the same risk & mastery quadrant. The Hero tries to prove their worth through courageous and difficult action while the Outlaw is focused on being a revolutionary for revolution sake. Each responds differently for different reasons. The health benefit plan that caters to these individual needs provides the greatest opportunity for appropriate behavior. The creator is more likely to respond to a smoking cessation program or wellness program. The caregiver will respond to general safety programs or incentives to get flu shots. The Ruler will respond more positively to a pre-authorization program.
Combined, personas and archetypes can be used to more effectively design health benefit programs to both attract the right type of individuals to the program and to indirectly impact how they make benefit and care decisions. Armed with the appropriate information, benefit plans can be uniquely designed on a group by group basis to positively impact health costs, improve profits and increase competitiveness of health plans.
So Where Do We Start?
There are several basic ingredients needed to develop a user-centric benefit design:
- Which providers are best able to provide high quality, cost-effective, patient centered care (requires provider profiling, assessing, ranking, care management assessments, etc.)? Who should we be sure are in our preferred networks? Analysis similar to that summarized below can be used to assess performance and compare to other providers.
- Which providers should be doing what care (i.e., stratification of care: basic care, intermediate care, tertiary/quarternary care)? How can benefits be defined to be sure these limitations are appropriately implemented? The following chart shows an example how DRGs can be allocated to the three types of care. Similar allocations can be done with all types of care helping to further stratify the benefit design process.
| Description | Base | Mid | Tertiary |
| Craniotomy Age > 17 w cc | x | ||
| Craniotomy Age > 17 w/o cc | x | ||
| Craniotomy Age 0 – 17 | x | ||
| No Longer Valid | |||
| No Longer Valid | |||
| Carpal Tunnel Release | x | ||
| Periph & Cranial Nerve & Other Nerv Syst Proc w cc | x | ||
| Periph & Cranial Nerve & Other Nerv Syst Proc w/o cc | x | ||
| Spinal Disorders & Injuries | x | ||
| Nervous System Neoplasms w cc | x | ||
| Nervous System Neoplasms w/o cc | x | ||
| Degenerative Nervous System Disorders | x | ||
| Multiple Sclerosis & Cerebellar Ataxia | x | ||
| Intracranial Hemorrhage or Cerebral Infraction | x | ||
| Nonspecific CVA & Precerbral Occlusion w/o Infract | x |
- What care management strategies should be pursued to manage different kinds of care in the most effective way (i.e., supply-sensitive care, preference-sensitive care, and quality/effective care) in light of the above provider selection and health care stratification? The chart below provides one example of this process.
| Stratification of Care | Classification of Care | ||
| Supply-Sensitive | Preference-Sensitive | Effective/Quality | |
| Basic | Manage network size, unit price focused (commodity), monitor performance, community connection | Information drive, comparative effectiveness study driven, providing provider current information on “best choices”, strong electronic connection with both providers and patients. Some need for authorization and confirmation of appropriate services | Strong primary care and wellness connection with patients, monitoring of essential quality services. |
| Intermediate | Centers of Excellence, quality-focused, monitor performance, strong focus on capacity/resource management | Emphasis on consistency, standardization, care planning, outcomes, etc. | |
| Tertiary/Quaternary | Center fo Excellence, quality/outcome focus, monitor performance | Emphasis on quality outcomes, monitoring of results, etc. | |
Once this information is known and the structure created, it can readily be merged with the personas and archetypes described earlier to determine what benefit structure best meets the unique needs of a particular population.
What Are the Key Steps?
Begin with a provider assessment where historical claim and eligibility information is analyzed to complete a thorough risk-adjusted provider profiling process. If patients are not directly assigned to primary care providers, patients are attributed to providers using simple attribution logic. Health costs are similarly assigned and risk-adjusted with ranked results developed showing which providers deliver the most efficient care. Geographic access analysis can be superimposed on this assessment to be sure adequate resources are identified by key geographic area. This analysis provides the framework to create the ideal provider network. We begin with assessing primary care providers, move on to specialists, hospitals and other types of providers. Each of the provider types would be associated with their respective health care costs using the actuarial cost model.
Health care costs would then be stratified by each of the care types (i.e., basic, intermediate, and tertiary/quaternary) and by the three care management classifications (i.e., supply-sensitive, preference-sensitive, and quality/effective care). This information provides a strategic matrix of health cost information than can be combined with the persona and archetype information for the population.
Broad information is also gathered across an entire population to better understand how individuals would behave.
Illustrative Health Care Persona and Archetype Categories
The studied population is then categorized by key persona categories. Some examples of persona categories that could be used are:
- Healthy low cost individuals – those with low risk scores and lower than average health care utilization and cost
- Chronic high cost/high risk individuals – serious ongoing conditions with higher risk scores
- Higher income/higher cost individuals
- Individuals consistently getting care from more efficient providers
- Individuals consistently getting care from less efficient providers
Persona and archetype information can be combined into clear patterns of making choices and decisions, including health benefit choices to help the plan designer attract and motivate the appropriate behavior. As individual members are assigned to specific persona/archetype categories with their underlying utilization and cost characteristics analyzed, valuable knowledge is gathered. Broad information is also gathered across an entire population to better understand how individuals would behave.
The Result
As information is gathered on each covered individual using both internal known information (i.e., demographics, income, health costs, health condition, etc.) and externally gathered information (i.e., consumer data, broad purchasing habits and choices, etc.) the individual can be categorized into a specific combination of persona and archetype. For a specific population, the individual characteristics can be combined into a single representation for that group with specific strategic benefit choice possibilities designed and offered to that group to provide the most ideal situation.
The plan variations can be standardized with a consistent, strategic and limited set of options for the specific marketplace. Certain market segments might have fewer options, others more. The needs of two different groups could be widely divergent, but the consistent application of the user-centric health benefit design approach would lead to more favorable results for the individual and the health plan.
A recent AHP Inspire article discussed the 24 benefit levers1 that could be used in benefit design to accomplish some of this targeted benefit design. This provides useful information for the benefit plan designer to achieve the results they desire.
Where Do We Go From Here?
As both health plans and plan sponsors seek improved solutions to their health cost crisis, this methodology can be used to refine or replace their current strategic model. No longer is benefit design limited to what increased deductible or cost sharing gets me to an acceptable premium rate using my traditional actuarial models. The user-centric health benefit design will identify a benefit design that enhances the customer experience, caters to the unique needs of the population while restraining the growth in health care costs and improving the affordability of health care.
1https://axenehp.com/the-24-lever-model-lowering-insurance-premiums/
About the Author

David Axene, FSA, FCA, CERA, MAAA, is the President and Founding Partner of Axene Health Partners, LLC and is based in AHP’s Murrieta, CA office.