Presented By:
Richard L. Liliedahl, MD
Erik D. Axene, MD
Oscar M. Lucas, ASA, FCA, MAAA
David V. Axene, FSA, FCA, CERA, MAAA
Over the past couple of weeks, COVID-19 has come upon both the American public and the healthcare community like a storm. As one of the cofounders of Axene Health Partners, LLC, a well-known health care consulting firm, I want to demonstrate our firm’s vital interest in the health and welfare of American families. As the firm’s Chief Medical Officer, I will introduce this topic and then share other perspectives from another physician and two actuaries who are part of the firm.
The Perspective of Richard L. Liliedahl, MD:
I share this initial information as a seasoned family practice physician of more than 40 years. During that time, I have never seen or experienced a pandemic of this sort. What astounds me the most has been the public responses regarding COVID-19. My multiple anecdotal and personal interactions from practicing physicians, Public health leaders, RNs from both California and Washington, laypeople and leaders of local organizations trying to create their COVID-19 policy show responses ranging from obstinate denial to extreme panic. This is likely the result of our collective lack of knowledge about this new and quickly emerging danger.
Some of my observations and related anecdotes:
- Young professionals from the technology industry discussing how they might try to get COVID-19, build immunity and then be available to help others during this crisis.
- Young man riding a bicycle with toilet paper piled high in front and obscuring his vision and then T-boning a moving car he didn’t see.
- Several leaders from mega-churches making decisions regarding the safety of attendees to their events on the now outdated CDC guidelines of meetings of less than 250 and not understanding the science of social distancing as the key issue.
- A smaller church with less than 250 still holding meetings because they assumed the number assured their safety.
- An RN stating with supposed firsthand knowledge that three children died at a nearby children’s hospital. This was later determined to be a rumor and not fact.
- Hospital leaders initially making all communication about this disease in their hospital confidential and hiding it from patients and others.
- Leaders making decisions to gather together in a group setting in a “macho manner” with indifference to the risk to them and others.
- Personal observation of long Costco lines, empty toilet paper and bottled water shelves in grocery stores and closing of public services
As I consider this information several related things come to mind:
- My medical school class where the first case study was about Dr. Semmelweis. Ignaz Semmelweis was a Hungarian physician practicing in Vienna. In 1846 he took an interest in puerperal sepsis and the death of the mothers. He figured out from data that male doctors and medical students had a rate of infection 5 times that of the female midwives. He theorized that the doctors were carrying something from the cadavers to the women in childbirth. He ordered chlorine handwashing by everyone and the sepsis rate fell. He was still not believed and remained an outcast. What was not known and not seen at that time killed thousands of people. Denial by the physicians killed thousands more. Dr. Semmelweis is known today as the Father of handwashing. This unseen microbe causing this sepsis is now known as Streptococci or Staphylococci[1].
- My time as a volunteer physician in Ghana, Africa in small villages treating children with malaria and dysentery. The mortality rate in children under 5 is primarily from these two diseases. They do not have clean drinking water and often walk three miles to obtain water from a contaminated pond. We installed clean water filters in their villages and instructed them on the dysentery risk and the death rate to the children from using that water. A year later the clean filter collection buckets where being used to carry the water and the filters became pots for plants. The education about unseen microbes is still a major issue today and takes many years to change. Many are working on that world-wide today. What the local villagers don’t know is still killing their children in that village and many parts of the third world.
- My experiences as I lived and practiced through the early stages of the HIV epidemic where little was known about the disease. National policy to physicians on transfusions at that time was very unclear. Physicians with limited understanding as myself were asked by patients about the safety of transfusions. At that time a minority of us advised against it with much pushback from colleagues. It was a difficult time for providers and patients with this limited knowledge and bad decisions were made impacting thousands[2]. It was many years before we understood this disease and today we have progressed to significant competency in understanding that disease.
The world today is much different with significant social and mass media and cellphone access around the world. But I would suggest there are lots of things about COVID-19 that are still unknown and the increase in misinformation has also become exponential. We are still in the early stages of learning about COVID-19. This contributes to both extreme anxiety and panic.
We are still in the early stages of learning about COVID-19. This contributes to both extreme anxiety and panic.
One of the best ways to look at and categorize our learning progress is the Broadwell Competence Model[3]. It is one way we can put into concrete terms how COVID-19 impacts the health care system and health care providers.
- Stage 1: Unconsciously incompetent and moving to Stage 2
- Stage 2: Consciously incompetent;
- Stage 3: Consciously Competent, and
- Stage 4: Unconsciously Competent.
Based upon this learning model I would suggest that as of today (3/18/2020) we are in Stage 1 since we don’t know much about what we don’t know including:
- What is the prevalence of COVID-19[4]? How many people in the US currently have the virus? More testing is to begin this week so additional learnings are just around the corner.
- Why is the US recovery rate so slow? In Washington State (the US epicenter) there are 904 cases, 1 recovered, 855 still active. Is this a timing issue?
- Can we really flatten the curve by social isolation[5]?
- What are the long-term costs of the disease and the sequelae such as chronic lung disease?
- Will this pandemic overwhelm our healthcare systems?
- How good is our data from foreign sources?
- When can we roll out broader testing and understand the prevalence?
- Can people who carry the virus 2 weeks after recovery still spread the disease[6]?
- What is the reinfection rate?It is not known yet. The SARs virus showed reinfection at 2 years.
- Will we have to ration ventilators? Italy had to ration ventilators based on who was most likely to survive.[7]
- As of 3/18/20 the millennial generation’s response, because of their high level of social activities and carrier rate, may be the most important factor[8]?
- Will we be able to find drugs that help patients until we have a vaccine[9]? For example, Chloroquine may work.
What we think we know at this time (Stage 2):
- Handwashing works[10]: credit Dr. Semmelweis as the father of handwashing.
- Peoples habits re: handwashing[11]: less than desired
- The virus lives on surfaces such as stainless steel up to 3 days[12]: its longer than expected
- Importance of social distancing[13]
- Corona is 2-3 times as contagious as flu and each infected person infects 2-3 others[14].
- The elderly are the most at risk[15]
- The current prevalence, death and recovery rates in US: based upon limited testing[16].
- We know we need to flatten the curve now![17]: we can’t wait!
Commentary: I believe we are at Stage 1 learning regarding COVID-19. In the Broadwell Competence Model, the greatest anxiety and stress occurs early in the Stage 2 level. I suggest our preliminary data puts us at this part of Stage 2. We are in the first month of this with public awareness at 10 – 14 days. It will be months before we move to Stage 3 or Stage 4 as it was with the Semmelweis and HIV epidemics stories. As the richest country in the world, with the best scientists and healthcare providers, we need to be at the forefront of this fight against COVID-19. We need to help the third world countries understand this disease and what they can do to save their fellow citizens.
The Perspective of Oscar Lucas, ASA, FCA, MAAA:
My uncle was a decorated combat veteran of the Korean War. One of his stories that stuck with me over the years seems to have an application to our current COVID-19 situation. During his time in Korea, many casualties were the result of enemy sniper activity. It seems that enemy snipers were targeting anything that created or reflected light, such as a metal mess kit, cup, watch or cigarette lighter. Improving your chances of survival required that soldiers quickly learn and follow “best practice guidelines” to avoid becoming a sniper’s target. These best practices were new and different from the way things were at home. But those who adapted quickly and made the practices into habits materially improved their chances of survival.
Today we are facing new challenges that require a different set of personal “best practices”. These are new and likely different from the way things were a few months ago before the emergence of COVID-19. Those who adopt these practices and make them personal habits will improve their own personal outcome as well as those around them.
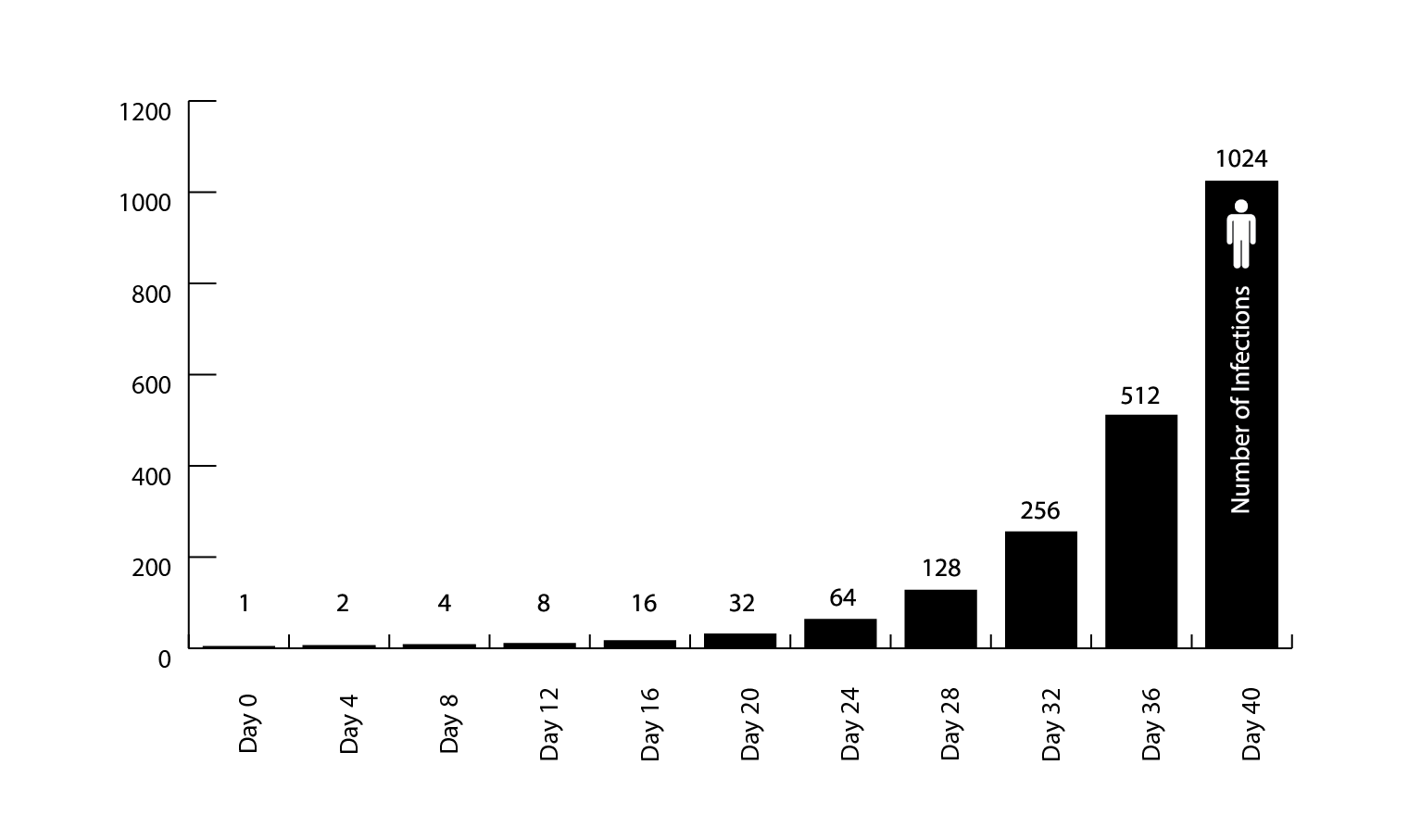
Understanding the math behind the spread of the COVID-19 virus is essential to understanding why recommended efforts to flatten the curve are important and why you should actively follow the recommended best practices. The World Health Organization (WHO) published as of March 15, the rate by country at which the number of confirmed COVID-19 cases are doubling. As of March 15, the U.S. rate was doubling every 4 days[18]. At this rate in 32 days, a single case has grown to 256 cases.
The U.S. is early in the pandemic with the first confirmed cases as of January 20th of this year. As testing and collection of data become more widespread, we may see revisions to the accuracy of this number. However, as long as there are available hosts (uninfected individuals) and individuals with active cases interacting or a vaccine become widely available, the number of cases will continue to rapidly grow.
The same WHO report shows China with a doubling rate as of March 15 of 34 days. This is significantly longer than the U.S rate of 4 days. For comparative purposes, a 34-day doubling rate would translate to 1 case at time zero becoming 2 cases in just over 1 month, compared to the US result of 256 cases. This is the result of containment efforts that have effectively flattened the growth curve and maturation of the virus’ impact on the Chinese population.
Commentary: Assume you are the first person at time zero. We can better understand how our actions might “break the chain” by avoiding or containing the spread of COVID-19, thereby impacting the lives of ourselves, our families and those around us. Whether you have the virus or not, your behavior can and will impact lots of people. We need to adopt best practices (see list at the conclusion) and develop consistent habits so that we can protect ourselves and others. Even though we are no longer at time zero, these practices are as important now as ever.
The Perspective of Erik D. Axene, MD:
Here are some of my thoughts regarding the foolish things I often hear in the ER:
- ER doctors tend to hope and prepare a lot. We hope for the best and prepare for the worst on every shift. We are hoping that the coronavirus doesn’t hit as hard as we fear, but we are preparing for the worst. I jumped at the opportunity to share my thoughts in this article and help spread accurate information about COVID-19. I see patients every day that have no idea they are contributing to the coronavirus pandemic and they are equally unaware that they can do something to be part of the solution.
- In my experience in the ER, patients who are contributing to the coronavirus pandemic are either flaunting a minimizing attitude or a fatalistic attitude toward the coronavirus. Minimizing patients will invariably tell me things like, “more people die of the flu every year, why should I be scared?” or “the media is blowing this way out of proportion! What do you think doc?” The more fatalistic patients will say things like “I’m going to get sick anyway so why worry?” If I had time to sit with these patients and tell them what I thought my waiting room would pile up, I would fall behind and potentially cause patient harm. So, I usually ignore these comments in sadness and move on to my next patient with a smile. Besides, my door-to-greet times and Press-Ganey (customer satisfaction) scores would take a nose dive if I stopped to set my obstinate patients straight. But if I didhave time to talk to these minimizers, I would pull out a whiteboard and teach them about the concept of the R0(pronounced “R nought”) and diagram out the differences in mortality rates between both viruses.
Here is a description of the last 24 hours in the life of this ER doctor in Texas.
This evening our internet went down. As a result, my emails were taking too long to load so I decided to drive my truck out into the driveway where I could get better reception on this rainy day in Texas. My daughter wanted to join me, so she sat there playing a game on her hand-held device while I read emails on mine. It was one of those special “daddy-daughter” moments, which lately are pretty rare. Emily, my daughter, soon asked me, “Daddy, what are you reading?” I started to answer but realized I couldn’t. If I tried to describe what I was reading it would either scare or confuse her, probably both. I answered instead, “Work stuff, sweetheart. What game are you playing?” While the rain gently fell on the canopy of my truck we continued to gently tap on our respective digital devices.
This particular email I was reading detailed out how we would triage patients if patient flow exceeded our ability to treat. Stated plainly, how do we decide who is worth saving? Sobered by the reality of what my job in the ER may soon become, I reflected on my last shift. It was a busy night shift with patient beds in the hallway, admits holding in the ER, and the ambulance phone ringing off the hook. At the beginning of my shift, I was greeted with three critically ill patients brought in by ambulance in a span of 16 minutes. The first ambulance brought me a very sick female in her 20s in a diabetic emergency called diabetic ketoacidosis. While attending to her the second ambulance brought me an unresponsive patient in her 60s needing emergent airway support. After placing this patient on a ventilator, the third ambulance brought me an elderly gentleman in cardiac arrest with paramedics performing CPR. Needless to say, I was grateful to my colleagues for seeing the slew of patients arriving through the front door at the same time. For later tonight I would not have the same luxury. I would be alone – an expected reality of an ER nocturnist.
In the not-too-distant future, critically ill patients such as these may be treated very differently. Here in the great State of Texas on St Patrick’s Day, all three of my patients ended up in the ICU and 2 of them on ventilators. On this St Patrick’s Day in Italy, my Italian ER and critical care colleagues may have treated these patients in a much different fashion. Perhaps the young diabetic would get resources as she is young and relatively healthy. But is there a ventilator for the 60-year-old female? Are there resources to care for the cardiac arrest patient with little chance of recovery? When supplies are limited, decisions such as this have tough answers.
The rain has now stopped and I have nearly caught up with my emails. I am now wondering about the patient’s I tested for coronavirus last night. Will they test positive? Have I been exposed? Am I in the middle of an incubation period? Will I spike a fever soon and join my quarantined colleagues? Just last week I was quarantined when a patient I treated was later found to be a PUI. I was not wearing a mask as I did not suspect her being a potential coronavirus patient. When I discovered that she was to be tested my heart sank. Fortunately, I was not working for a few days and did not have to find a doctor to replace me. With estimates of 2-3 days for test results, I prepared for being out of contact from my family. Fortunately, the patient tested negative and the quarantine was lifted. This is the new reality of life in the hospital.
There are no more unread emails in my inbox. My daughter and I have parked the truck back in the garage. It is time to enjoy dinner before another night shift. I wonder how many coronavirus tests I will order tonight. It is nice to know that I will likely have resources to treat any critically ill patient that enters my ER. It is nice to know that I will likely have ICU beds and ventilators available. I think of my ER colleagues in other hospitals practicing medicine with limited supplies overrun by the coronavirus. As I intubate my next elderly patient, I will be mindful of my ER colleagues handing a family a home palliative care plan as they have run out of ventilators.
Commentary: I recently received an email from a very intelligent friend of mine who likened the coronavirus to the atomic bomb and sent me a quote from CS Lewis in 1948 in his article “On Living in an Atomic Age”:
This is the first point to be made: and the first action to be taken is to pull ourselves together. If we are all going to be destroyed by an atomic bomb, let that bomb when it come find us doing sensible and human things—praying, working, teaching, reading, listening to music, bathing the children, playing tennis, chatting to our friends over a pint and a game of darts—not huddled together like frightened sheep and thinking about bombs. They may break our bodies but they need not dominate our minds.
I have a problem with this comparison of the coronavirus to the Atomic bomb. And I think this is part of the problem in our country. First of all, I happen to agree that fear is not going to solve any problems, so I find endeavoring in this activity quite counterproductive. I also agree that we should find a way to bolster up the human spirit and experience life in the midst of adversity and find joy in living regardless of circumstances. What I have a problem with is that there is little anyone could do to change whether or not an Atomic bomb was dropped. Today we are the Atomic bomb collectively. The very definition of a virus (thanks to google) makes my point.
A virus is an infective agent that typically consists of a nucleic acid molecule in a protein coat, is too small to be seen by light microscopy, and is able to multiply only within the living cells [italics added].
A virus is totally dependent on living things. It cannot survive otherwise. This infective agent (microscopic atomic bomb, if you will) depends on its host to live. We may be powerless when it comes to atomic bombs being dropped but we are not powerless to interfere with the lifecycle of the coronavirus that is threatening our way of life globally. We may not be able to stop this virus from spreading but we can decrease the rate of spread and minimize its damage.
Instead, I see most people disregarding recommendations and advisories from the CDC or the WHO while they continue to live their lives. In fact, I have heard people say, “I need to take this vacation now before we get quarantined!” Of the many things you can do to slow this virus down, social distancing is one. It was a smart move to cancel the NBA, MLB, XFL and NHL seasons. Large human gatherings increase the frequency of human contact and thereby virus transmission.
Your personal decisions and personal hygiene could literally save millions of lives. Think about that for a minute.
Some have said of “social distancing” that it is an un-loving promotion of isolation. Isolation happens to be a great way to love our neighbors, this temporary practice of social distancing interferes with the propagation of the coronavirus. We need to discipline ourselves to fight against this virus. We do this by working together as a community of people following the recommendations of some of the smartest people on the planet.
Wash your hands frequently, don’t touch your face, cough/sneeze into the nape of your elbow, be steadfast in your practice of social distancing and we might, just might, have a chance to slow this thing down enough to minimize its effect on our country’s healthcare system. Your personal decisions and personal hygiene could literally save millions of lives. Think about that for a minute.
Commentary from AHP Managing Partner David Axene, FSA, CERA, FCA, MAAA:
You have heard from three leading experts on what we as a nation and frankly world are experiencing. It is obvious we need to learn more, but more obvious that we need to take immediate action to preserve life as we now know it. We might have valid concerns about the reliability of some of the data we see and what our leaders are asking us to do, but we need to listen.
Be grateful that you are not in a third world country about to be ambushed by something you will not understand. Do what you can to not become the individual who infects the next 1,000 individuals. Today we are where Italy was two weeks ago[19].
Final commentary from Dr. Liliedahl: My daughter-in-law is working in a hospital unit with 5 active cases. I told her that she and others like her and my son working in the same hospital are the real American heroes and I would be praying for them and my grandchildren. Suddenly this has become very personal for me. I think we should as all Americans focus on flattening the curve now and hope we’re wrong!
Social isolation is the best way to love our neighbors at this time!
- Wash your hands frequently
- Don’t touch your face
- Cough into your elbow or a tissue
- Practice social distancing.
- Your personal decisions and hygiene could impact 1000s
- One infection becomes 1000 in less than 40 days
Endnotes
[2] https://www.ncbi.nlm.nih.gov/books/NBK232419/
[3] https://en.wikipedia.org/wiki/Four_stages_of_competence
[4] https://www.ncbi.nlm.nih.gov/books/NBK232419/
[6] https://www.livescience.com/coronavirus-spread-after-recovery.html
[8] https://ktla.com/news/coronavirus/white-house-warns-millennials-stay-out-of-bars-during-outbreak/
[9] https://www.thechronicle.com.au/news/cure-found-for-coronavirus-in-australia/3973564/
[10] https://www.webmd.com/lung/what-is-covid-19#1
[11] https://msutoday.msu.edu/_/pdf/assets/2013/hand-washing-study.pdf
[13] https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html
[15] https://www.statista.com/chart/20860/coronavirus-fatality-rate-by-age/
[16] https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
[17] https://www.foxnews.com/us/when-will-coronavirus-peak-in-the-us-flattening-the-curve
[19] https://www.foxnews.com/us/when-will-coronavirus-peak-in-the-us-flattening-the-curve
Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.