The Affordable Care Act (ACA), colloquially known as “Obamacare”, recently began its 7thopen enrollment period, the first with premiums based on claims experience after the 2018 Cost Sharing Reduction (CSR) payments were defunded. Despite seven years of experience and three years after the paradigm shift of 2018, many of the ACA’s non-intuitive mechanics and incentives are still misunderstood to this day. It’s always helpful to start with the two major outcomes of the law; the lowering of the uninsured rate and the protection of those with pre-existing conditions.
Lowering the uninsured rate was primarily accomplished through expanding Medicaid[1] to low-income adults and to a lesser degree assuring large employers will cover healthcare via the employer mandate. The third leg of lowering the uninsured rate had the dual purpose of protecting those with pre-existing conditions. This third leg was the establishment of federally subsidized, community-rated, partial high-risk pools in each state known as the individual market. The individual market guaranteed coverage regardless of health status and served as the vehicle for over $55 billion of premium subsidies[2] which assured people would enroll and insurance companies would participate.
The individual market is a fascinating case study of how incentives drive consumers while also creating unintended consequences. As the individual market is comprised of over 66% subsidized enrollees[3], its functionality is largely driven by how subsidies are distributed. The greater the subsidies, the greater the enrollment and the better the risk. With that in mind, I decided to create a market optimization equation to evaluate how each state has done in terms of maximizing the potential value to individual market consumers. The point of the state rankings is to help describe what drives consumer value in the individual market as well as point to areas of improvement that many states can further understand. Plus, rankings of any kind are just fun in general.
I chose four value categories and gave them equal weight. For every state, each value category is given a value score ranging from 1 (worst value) to 5 (best value) with linear interpolation between 1 and 5. The four categories are then combined and every state is given a final value score. I describe the four value categories below which is then followed by the state ranking.
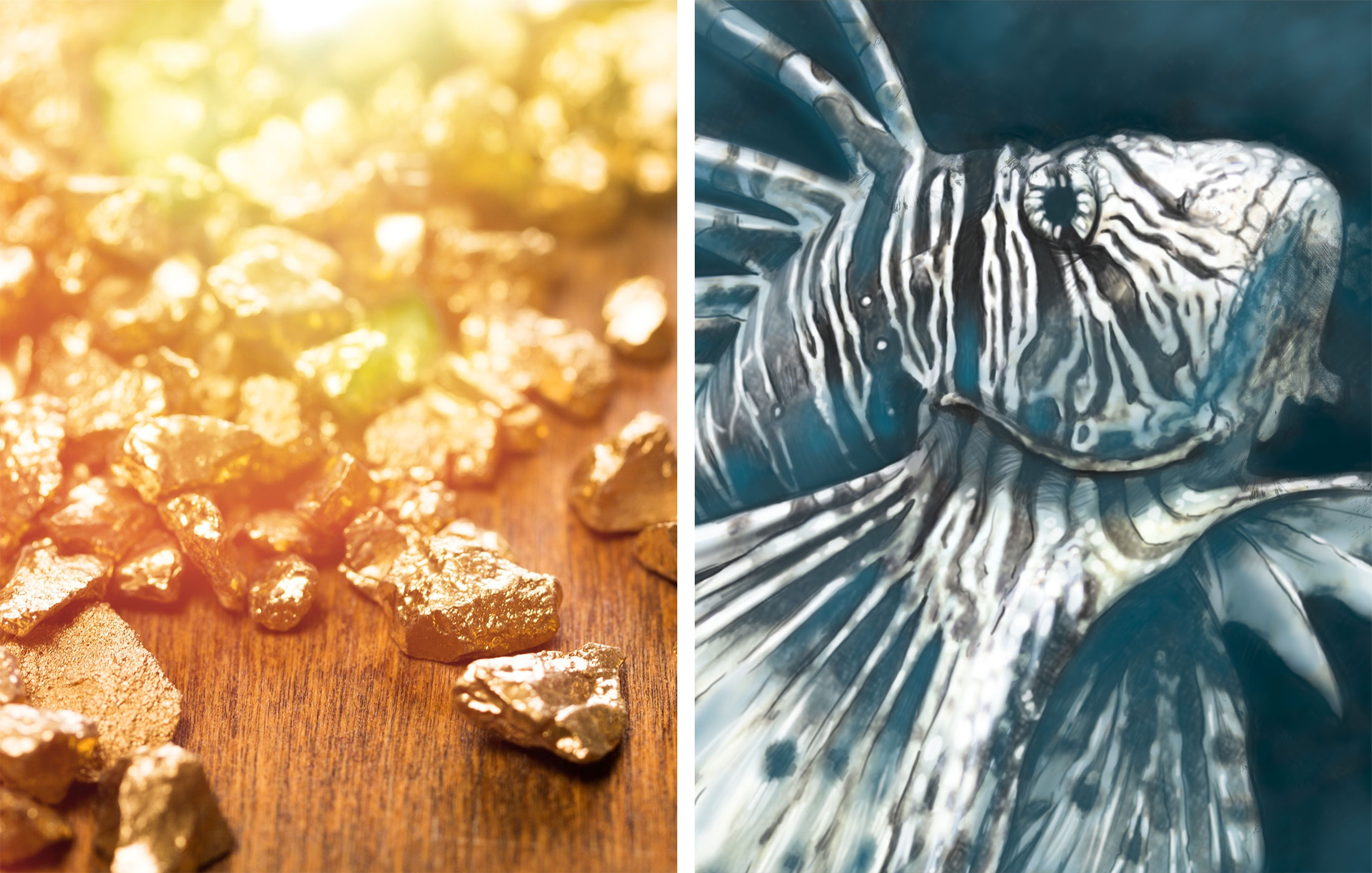
1st Value Category: Gold to Silver Premium Ratios
Description of Metric: When I die they may put on my tombstone, “here lies Daniel Cruz, he claimed Gold is less than Silver”. Due to the Trump administration’s defunding of Cost Share Reduction (CSR) payments to insurance companies in 2018[4], on-exchange Silver premiums are now based on a mixture of platinum-level benefits received by CSR eligible enrollees and silver-level benefits from non-CSR enrollees. Platinum-level, CSR enrollment is close to 75% for on-exchange Silver enrollees which means Silver premiums should look more like traditional Platinum than Silver premiums. Silver premiums are expected to be equal to or greater than Gold premiums, the middle point between Silver and Platinum. The pricing mechanics of this are complicated as explained by Greg Fann who explored the CSR impact in 2017, https://axenehp.com/cost-sharing-reduction-paradox-defunding-help-aca-markets-not-make-implode/, and an article co-written by myself and Fann about the surprising disparities between actual state responses compared to expectations, https://axenehp.com/fields-of-gold/. From Fann’s article, the following table visually describes the expectations in a CSR defunded market.
Metric Used: Average Gold to Silver pricing factors weighted by carrier enrollment for each state. The pricing factors are available for the first time on the 2020 URRT public use file[5].
Why it Matters to Consumers: Subsidies are based on the second lowest cost Silver (benchmark) premiums available to the consumer. If you choose a plan that’s higher than the benchmark you must pay every dollar above the benchmark and if you choose a plan lower than the benchmark, then you pay less by every dollar below the benchmark. Prior to 2018, this made the relative cost of Gold plans out of reach for most low-income individuals (non-CSR), leaving them incentivized to select higher deductible plans. Post 2018, the rules were expected to result in Gold being equal to or less than the benchmark plan meaning for the first time in ACA history, low-income consumers (non-CSR) would be incentivized to select low deductible plans. However, most states have allowed outlier rating relationships between Gold and Silver premiums and Gold plans remain out of reach for low-income enrollees in most states. This reflects a market failure that can be corrected by regulators through stricter rate review[6] which can result in better coverage for non-CSR subsidized consumers. All the mining tools are available for states to initiate the gold rush and avoid fool’s gold in their market. This value score reflects whether the state has leveraged the increased opportunity created by the Trump Administration’s actions in 2018. This score also reflects state actions past or present that don’t allow the state to leverage the 2018 market change such as the Basic Health Programs or states that did not allow silver loading.
Value Scoring:
| Gold to Silver Premium Ratios Value Scoring | ||
| Value Ranking | Value Score | Gold to Silver Premium Ratio |
| Gold Rush | 5 | < = 100% |
| Keep Diggin | 3-4 | 100% - 110% |
| Fool's Gold | 1-2 | > 110% |
2nd Value Category: Lionfish Penetration
Description of Metric: Who knew healthcare slang and analogies were so creative? The ACA has produced wonders such as Silver Loading, family-glitch and grandmothered plans just to name a few. Thanks to my colleague Greg Fann we have a new term he coined, the Lionfish in ACA markets. Back to incentives and unintended consequences, tying the subsidies to the second lowest cost Silver plan means you will get significantly less enrollment the higher you are compared to the benchmark. If a low-cost plan enters the waters of a given market, then the benchmark is reduced, the subsidies are reduced, and the higher cost plans are pressured to react by making more competitive products aka more restrictive networks. This is obviously not an ideal outcome for subsidized consumers as they pay the same amount but get less value through more narrow network plans.
So what exactly is a Lionfish plan? A Lionfish plan is defined as a plan that is both non-native to the commercial waters and is significantly cheaper than a standard baseline commercial plan. Non-native is defined as a carrier that does not significantly participate in the employer market or specific networks of carriers that are native but are significantly cheaper than their full network plan. “Significantly cheaper” was defined as being at least 10-15% cheaper on average than a standard baseline product in the market. And what is a Lionfish? In Greg’s own description:
“It’s a fish that behaves like a fish. It causes few problems in its native environment. It may even comfortably adjust to new environments as well. The problem is the havoc it causes when introduced to an ecosystem it should not be in. It is what the scientific community calls an invasive species”. https://axenehp.com/lionfish-aca-markets/
Metric Used: For federal exchange states, the % of counties, weighted by county population, that have a Lionfish plan as the benchmark plan. For state-based exchange states, the % total market share of Lionfish plans using 2020 projected member months from the 2020 URRT for plans sold on exchange.
Why it Matters to Consumers: It’s not enough to simply look at the cost of a health plan to determine value. The product itself needs to be evaluated. When comparing the individual market to the employer market in each state, the presence of a Lionfish plan as the benchmark means individual market subsidized consumers must pay significantly more to purchase a standard commercial plan typically available to their fellow statesman receiving coverage in the employer market. In a sense, low-income individuals are driven by the subsidy mechanics to purchase either narrow network plans or networks that are typically available to Medicaid populations when these Lionfish plans exist. It should be noted that some non-native plans from carriers traditionally participating as Medicaid managed care plans[7] do add value and have in the past provided stability in markets where large commercial health plans exited.
In terms of value, they provide continuity of care for those transitioning to and from the individual market to Medicaid. Secondly, if they are the lowest cost plan and not the benchmark, they provide even lower net premiums for CSR enrollees and others. And lastly, they are a low-cost option for the unsubsidized, though unsubsidized are less likely to select them. While it’s not entirely clear that the transitional enrollees wouldn’t prefer a non-Medicaid network, it is clear that Lionfish plans negatively reduce subsidies, increase net premiums for subsidized enrollees and drive consumers into more narrow networks. It is therefore a net negative to subsidized enrollees to have a Lionfish lurking in the waters of their ACA market.
Value Scoring:
| Lionfish Penetration Value Scoring | ||
| Value Ranking | Value Score | Lionfish Penetration |
| Clear Waters | 5 | 0% |
| Lionfish Sighting | 3-4 | 1% - 50% |
| Lionfish Invasion | 1-2 | > 50% |
3rd Value Category: Average Subsidized (Net) Premium
Description of Metric: The prior two categories help explain why subsidized and unsubsidized premiums may be higher or lower but there is no one to one relationship as it depends on how many carriers are competing in each area, what plans are offered and who is the benchmark. Downstream of all that is the actual financial impact to consumers. This category reflects the average lowest cost net premiums (after subsidies) available for Bronze, Silver and Gold subsidized enrollees.
Metric Used: Lowest cost Bronze, Silver and Gold net premiums weighted by county population. An average of the three net premiums was used as an overall metric for each state. The rates were for a 40-year-old making 300% of the FPL.[8]
Why it Matters to Consumers: We have a lot of convoluted conversations about the ACA on many topics. At the end of all that are low-income individuals trying to get coverage for themselves and their families. This matters a lot and a $100 difference a month can help or hurt low-income families. The financial impact is the bottom line of the ACA where, after all, the first letter of the law stands for “Affordable”.
Value Scoring:
| Average Subsidized Premium Value Scoring | ||
| Value Ranking | Value Score | Average Subsidized Premium (40 Year Old), 300% of FPL |
| $ | 2.8 - 5.0 | < $235 |
| $$ | 1.5 - 2.8 | $235 - $295 |
| $$$ | < 1.5 | > $295 |
4th Value Category: Average Gross Premium
Description of Metric: Like net premiums this is a downstream financial value category for the consumer. This category reflects the lowest cost gross premiums available for Bronze and Gold unsubsidized enrollees. Silver was excluded because on-exchange Silver is loaded to reflect Platinum level benefits and no unsubsidized enrollee should ever purchase on-exchange Silver plans. This category reflects actual costs in each market which is a mixture of health plans available, networks available, morbidity of the risk pool, level of managed care in the market, state efforts to reduce costs like 1332 waivers along with many other factors.
Metric Used: Lowest cost Bronze and Gold gross premiums weighted by county population. An average of the two gross premiums was used as an overall metric for each state. The rates were for a 40-year-old making more than 400% of the FPL.[9]
Why it Matters to Consumers: Consumers making above 400% of the FPL receive no federal subsidy assistance to purchase coverage. These consumers face extremely high costs in the post ACA individual market which is the negative aspect of covering pre-existing conditions. The higher the costs, the more likely these consumers will seek care elsewhere in non-major medical plans or simply go without coverage. The unsubsidized consumers represent about one third of the market and as such significantly contribute to the overall risk pool. The lower the gross cost, the greater the enrollment of unsubsidized, the lower the risk of the unsubsidized.
Value Scoring:
| Average Unsubsidized Premium Value Scoring | ||
| Value Ranking | Value Score | Average Unsubsidized Premium (40 Year Old) |
| $ | 4 - 5 | < $375 |
| $$ | 2 - 3 | $375 - $490 |
| $$$ | < 2 | > $490 |
State Ranking
The following table displays the results of my analysis and value scoring. Each category is meant to balance out each other as some value improvements in one direction result in the non-intuitive decrease in value in the other direction. For instance, lower cost health plans improve value for the unsubsidized who bear the full cost but decreases value for the subsidized who receive lower subsidies. The states are also grouped by color code with dark green representing the states with the greatest optimization of value, light green the states with fair optimization, yellow with poor optimization and red being the least optimization.
As an actuary, I would like to point out the opportunity on the table for those in my profession. Silver on-exchange plans should be chosen by only individuals making under 200% of the FPL who don’t receive the actual silver benefits. Prisoner Dilemma[10] for the carriers aside (and federal tax expenditures), there is no market wide upside to compressing Silver premiums in relation to other metal levels. The rules are in place to maximize subsidies and to leverage current rules to force carriers to compete on Gold plans, thereby delivering highly subsidized low-cost sharing plans to low-income individuals in the market. Actuaries, both regulators and pricing, the ball is in our court for 2021 to improve the market.
| Optimization State Rank | State | Gold to Silver Premium Ratios | Lionfish Penetration | Average Subsidized Premiums | Average Unsubsidized Premiums | Overall State Value Score |
|---|---|---|---|---|---|---|
| 1 | IA | Gold Rush | Clear Waters | $ | $$ | 4.39 |
| 2 | MD | Gold Rush | Clear Waters | $$ | $ | 4.38 |
| 3 | OK | Gold Rush | Clear Waters | $ | $$ | 4.20 |
| 4 | ND | Gold Rush | Clear Waters | $$ | $ | 4.19 |
| 5 | NM | Keep Diggin | Lionfish Sighting | $$ | $ | 4.04 |
| 6 | WY | Gold Rush | Clear Waters | $ | $$$ | 3.88 |
| 7 | DE | Keep Diggin | Clear Waters | $ | $$ | 3.85 |
| 8 | KS | Gold Rush | Clear Waters | $$ | $$ | 3.84 |
| 9 | VA | Gold Rush | Clear Waters | $$ | $$ | 3.83 |
| 10 | HI | Gold Rush | Clear Waters | $$$ | $$ | 3.67 |
| 11 | ID | Keep Diggin | Clear Waters | $$ | $$ | 3.62 |
| 12 | NC | Keep Diggin | Lionfish Sighting | $ | $$ | 3.61 |
| 13 | CT | Keep Diggin | Clear Waters | $ | $$ | 3.60 |
| 14 | MT | Keep Diggin | Clear Waters | $$ | $$ | 3.49 |
| 15 | OR | Fools Gold | Clear Waters | $$ | $$ | 3.48 |
| 16 | NE | Gold Rush | Lionfish Sighting | $ | $$$ | 3.47 |
| 17 | RI | Keep Diggin | Lionfish Invasion | $$ | $ | 3.44 |
| 18 | VT | Keep Diggin | Clear Waters | $ | $$$ | 3.41 |
| 19 | AK | Gold Rush | Clear Waters | $$ | $$$ | 3.35 |
| 20 | PA | Keep Diggin | Lionfish Sighting | $$ | $$ | 3.27 |
| 21 | CO | Fools Gold | Clear Waters | $$ | $ | 3.26 |
| 22 | SC | Keep Diggin | Lionfish Sighting | $$ | $$ | 3.25 |
| 23 | FL | Keep Diggin | Lionfish Sighting | $$ | $$ | 3.14 |
| 24 | CA | Fools Gold | Lionfish Sighting | $ | $$ | 3.10 |
| 25 | NH | Fools Gold | Clear Waters | $$ | $$ | 2.99 |
| 26 | SD | Keep Diggin | Clear Waters | $$ | $$$ | 2.95 |
| 27 | MI | Fools Gold | Lionfish Invasion | $$ | $ | 2.93 |
| 28 | MN | Fools Gold | Lionfish Sighting | $$$ | $ | 2.93 |
| 29 | NV | Fools Gold | Clear Waters | $$$ | $$ | 2.83 |
| 30 | MA | Fools Gold | Lionfish Sighting | $$ | $ | 2.83 |
| 31 | DC | Fools Gold | Clear Waters | $$ | $$ | 2.81 |
| 32 | AR | Fools Gold | Clear Waters | $$$ | $$ | 2.80 |
| 33 | WI | Fools Gold | Lionfish Sighting | $$ | $$ | 2.73 |
| 34 | WA | Fools Gold | Lionfish Invasion | $$ | $ | 2.70 |
| 35 | LA | Fools Gold | Lionfish Sighting | $$ | $$ | 2.70 |
| 36 | UT | Fools Gold | Clear Waters | $$ | $$ | 2.68 |
| 37 | IL | Fools Gold | Lionfish Sighting | $$ | $$ | 2.62 |
| 38 | ME | Fools Gold | Clear Waters | $$ | $$$ | 2.60 |
| 39 | AL | Fools Gold | Clear Waters | $$ | $$$ | 2.52 |
| 40 | TX | Fools Gold | Lionfish Invasion | $$ | $$ | 2.49 |
| 41 | GA | Fools Gold | Lionfish Invasion | $$ | $$ | 2.39 |
| 42 | OH | Fools Gold | Lionfish Invasion | $$ | $ | 2.36 |
| 43 | AZ | Fools Gold | Clear Waters | $$$ | $$ | 2.34 |
| 44 | NY | Fools Gold | Lionfish Sighting | $$ | $$$ | 2.17 |
| 45 | TN | Fools Gold | Lionfish Sighting | $$ | $$ | 2.01 |
| 46 | KY | Fools Gold | Lionfish Invasion | $$ | $$ | 1.83 |
| 47 | NJ | Fools Gold | Lionfish Invasion | $$$ | $$ | 1.64 |
| 48 | IN | Fools Gold | Lionfish Invasion | $$$ | $$ | 1.56 |
| 49 | MO | Fools Gold | Lionfish Invasion | $$$ | $$$ | 1.48 |
| 50 | MS | Fools Gold | Lionfish Invasion | $$$ | $$$ | 1.31 |
| 51 | WV | Fools Gold | Lionfish Invasion | $$$ | $$$ | 1.21 |
State Groupings
The following represents groupings of states that may provide some interesting insights. The groupings are different state actions which were mostly aimed at reducing overall costs in the individual market. An average value score for each value category was calculated for each group. None of the overall value equations can be directly attributed to the direct actions of the groupings, rather, these groupings are useful in measuring how the different categories are affected with the financial categories of subsidized and unsubsidized costs being most directly impacted. The average overall state value scores are equal to 2.98 when averaging all 50 states plus DC.
| Category | Gold to Silver Premium Ratios | Lionfish Penetration | Average Subsidized Premiums | Average Unsubsidized Premiums | Overall State Approval Score |
| State Exchange | 2.57 | 4.22 | 2.15 | 3.68 | 3.16 |
| Federal Platform | 2.97 | 3.76 | 2.16 | 2.80 | 2.92 |
| 1332 Waivers | 2.82 | 4.12 | 1.97 | 3.15 | 3.01 |
| No 1332 Waivers | 2.88 | 3.56 | 2.19 | 3.00 | 2.98 |
| Medicaid Expansion | 2.82 | 4.00 | 2.07 | 3.25 | 3.04 |
| No Medicaid Expansion | 2.98 | 3.56 | 2.40 | 2.42 | 2.84 |
| State Individual Mandate | 2.61 | 3.37 | 2.08 | 3.43 | 2.87 |
| No State Individual Mandate | 2.90 | 3.95 | 2.17 | 2.97 | 3.00 |
| Limits on Short Term Plans | 3.18 | 4.23 | 2.17 | 3.41 | 3.25 |
| No Limits on Short Term Plans | 2.61 | 3.59 | 2.16 | 2.70 | 2.77 |
| Gold Rush States | 5.00 | 4.84 | 3.06 | 2.78 | 3.92 |
| Non Gold Rush States | 2.35 | 3.65 | 1.94 | 3.08 | 2.75 |
| No Lionfish States | 3.35 | 5.00 | 2.36 | 2.89 | 3.40 |
| Lionfish States | 2.41 | 2.80 | 1.97 | 3.15 | 2.58 |
Most results follow expectations with state actions increasing value for the unsubsidized by lowering overall costs but decreasing value for the subsidized by also lowering subsidies. The greatest value improvement for the subsidized premiums can be found in the “Gold Rush” states which have a 3.06 value compared to 1.94 for non “Gold Rush” states. The greatest value improvement for the unsubsidized premiums can be found in the “State Exchange” states which have a 3.68 value compared to 2.80 for “Federal Platform” states.
Endnotes
[4]https://axenehp.com/obamacares-unlikely-savior/
[5]From Worksheet 2, field name ADJ_FACT_AV_CS. 2020 URRT PUF: https://www.cms.gov/CCIIO/Resources/Data-Resources/marketplace-puf
[6]https://axenehp.com/making-rate-review-great/
[7]https://www.healthaffairs.org/do/10.1377/hblog20180823.490433/full/
[8]2020 California state subsidies were included in the analysis. Federal Exchange states, actual 2020 premiums by county were used and weighted by county. For State based exchange states, the following study was used: https://www.kff.org/health-reform/state-indicator/average-marketplace-premiums-by-metal-tier/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7
[9]See note on subsidized methodology.
[10]The Prisoner’s Dilemma is a situation in which every player has the best result if everybody chooses A but individually, they receive the worst outcome if they choose A and the rest choose B. Therefore, they all choose B which gives them average results.

Any views or opinions presented in this article are solely those of the author and do not necessarily represent those of the company. AHP accepts no liability for the content of this article, or for the consequences of any actions taken on the basis of the information provided unless that information is subsequently confirmed in writing.